Ultimate Guide to Teen Bedwetting Solutions

Teen bedwetting, or nocturnal enuresis, affects many families and can be stressful for both teens and parents. It’s commonly caused by delayed brain-bladder communication, genetics, or medical conditions like sleep apnea or urinary tract infections. Emotional stress and lifestyle habits, such as excessive fluid intake before bed or irregular sleep schedules, can also contribute.
Key Takeaways:
-
Types of Bedwetting:
- Primary: Ongoing since childhood.
- Secondary: Reappears after 6+ months of being dry, often linked to medical or emotional triggers.
-
When to See a Doctor:
- If bedwetting happens twice a week for 3+ months.
- If accompanied by pain, daytime accidents, or other symptoms (e.g., fever, extreme thirst).
-
Management Strategies:
- Establish consistent nighttime routines (e.g., double voiding, limiting fluids before bed).
- Use bedwetting alarms to train the brain to wake up when the bladder is full.
- Protective bedding like PeelAways disposable sheets simplifies cleanup and reduces stress.
- Medications, such as desmopressin, can help in certain cases.
-
Emotional Support:
- Avoid blame or punishment.
- Maintain privacy and involve teens in managing their condition.
Bedwetting is manageable with the right mix of medical guidance, practical tools, and emotional support. Most teens grow out of it naturally, but persistent cases may require professional evaluation.
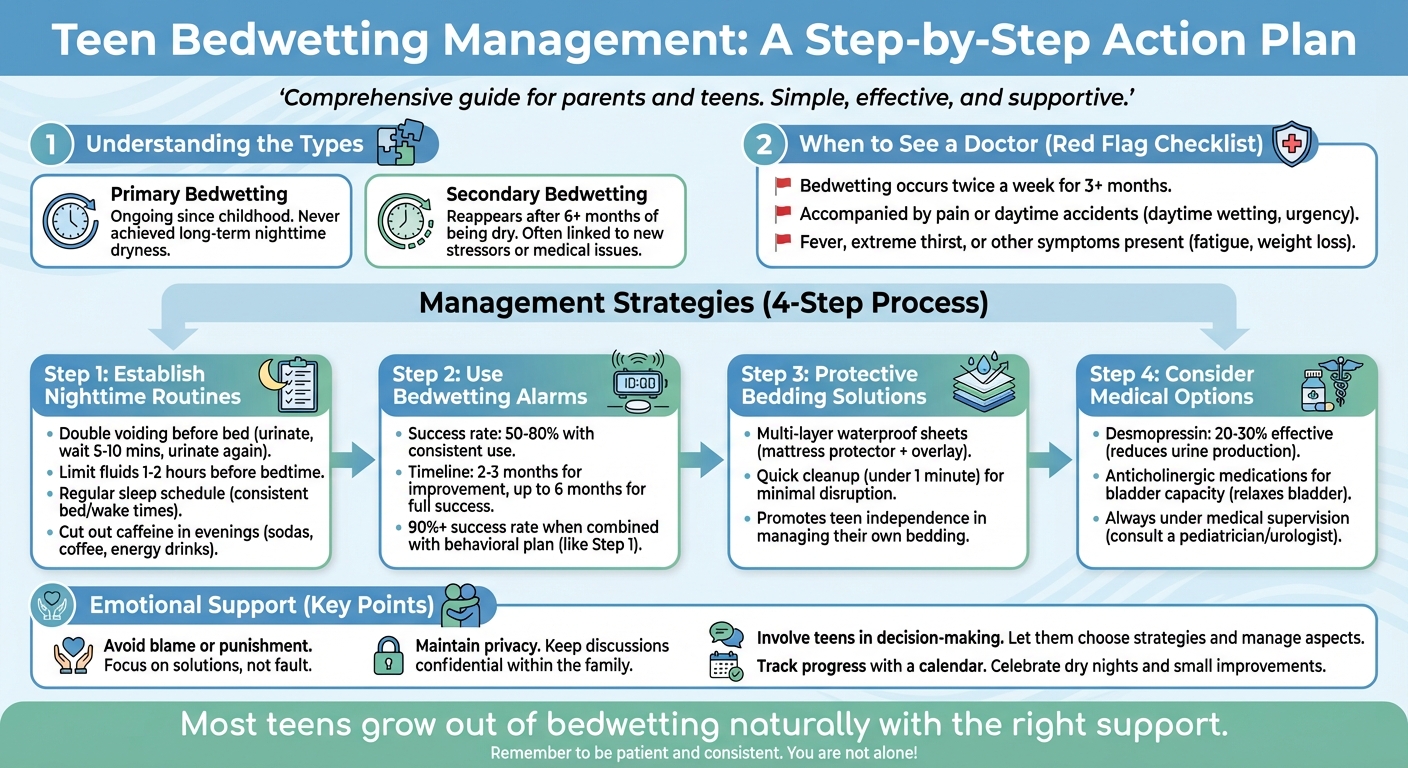
Teen Bedwetting Management: A Step-by-Step Action Plan
Child & Teenage Bedwetting Treatment Options
What Causes Teen Bedwetting
Teen bedwetting stems from a combination of physical and emotional factors. Unlike younger children, teens often face a more intricate mix of causes.
Medical Causes
Genetics often plays a big role in teen bedwetting. If one parent experienced bedwetting as a child, their teen is at a higher risk; if both parents did, the likelihood increases significantly. This genetic link can influence nighttime urine production, bladder capacity, and how easily the brain responds to a full bladder during sleep.[3][5]
Hormonal imbalances, particularly low levels of antidiuretic hormone (ADH) at night, can also be a factor. ADH typically signals the kidneys to produce less urine during sleep, but when levels are insufficient, the bladder may fill beyond its capacity. Families might notice very wet sheets or large amounts of urine when accidents happen.[5][7]
Deep sleep patterns are another contributing factor. Teens who are heavy sleepers may not wake up when their bladder signals the need to empty. If your teen struggles to wake up in the morning or sleeps through alarms, this could be part of the issue. Additionally, obstructive sleep apnea (OSA) can make the situation worse by disrupting breathing during sleep, which affects body chemistry and increases nighttime urine production. Signs of OSA include loud snoring, mouth breathing, restless sleep, and excessive daytime tiredness.[1][5]
Other medical conditions linked to bedwetting include urinary tract infections (causing symptoms like pain, burning, or cloudy urine), diabetes (characterized by extreme thirst and frequent urination), and constipation, where backed-up stool can press on the bladder. Rarely, bladder, kidney, or neurological problems may be involved, especially if daytime symptoms are present as well.[1][3][5]
Psychological and Lifestyle Factors
In addition to medical causes, emotional stress and lifestyle habits can influence bedwetting. While emotional factors alone rarely cause bedwetting, they can exacerbate the problem in teens who are already susceptible.[4][5][8] For instance, secondary bedwetting - when a teen who had been dry for at least six months starts wetting the bed again - often coincides with stressful events like family conflicts, divorce, moving, changing schools, exam stress, or bullying. Stress can disrupt sleep, affect hormone levels, and impair bladder function, all of which make nighttime control more challenging.[4][8]
Day-to-day habits also play a role. Drinking too much liquid close to bedtime can overwhelm the bladder, while caffeine from sodas, energy drinks, or coffee stimulates urine production and irritates the bladder.[6] Irregular sleep schedules and staying up too late can leave teens overtired, making it harder for them to wake when their bladder is full.[3][5][6] A diet lacking in fiber, combined with insufficient water intake during the day, can lead to constipation, which reduces bladder capacity by putting pressure on it.[3][5][8]
When to See a Doctor
If your teen is wetting the bed regularly (at least twice a week for three months or more), it’s a good idea to consult a healthcare provider, as most teens are dry by this age.[2][4] Secondary bedwetting should always be evaluated, as it may indicate underlying medical or emotional issues.[1][4]
Seek medical attention promptly if your teen has daytime bladder issues like frequent or urgent urination, leaks during the day, or pain when urinating. Other warning signs include symptoms of infection (fever, back pain, or unusual urine), possible diabetes (excessive thirst, weight loss), or sleep-disordered breathing (loud snoring, gasping, or pauses in breathing). Numbness, tingling, leg weakness, or changes in walking patterns should also be checked immediately, as these may point to neurological concerns.[1][5][8]
Understanding these causes sets the stage for discussing effective management strategies in the next section.
Practical Solutions for Managing Teen Bedwetting
Once you’ve identified what might be contributing to your teen’s bedwetting, the next step is implementing practical strategies. These can help simplify nighttime routines while preserving their dignity and fostering independence.
Nighttime Routines and Preparation
Consistency makes a big difference. Setting a regular sleep schedule - going to bed and waking up at the same time daily - can help regulate your teen’s internal clock. Encourage them to stay well-hydrated throughout the day but limit fluids in the 1–2 hours before bedtime. Double voiding, or using the bathroom both before starting the bedtime routine and again right before sleep, can also reduce accidents. Cutting out caffeine and sugary drinks in the evening is another way to minimize nighttime urine production.
Adding small night lights in hallways or bathrooms makes nighttime trips easier and safer. Some families even use a scheduled alarm during the night to prompt an additional bathroom visit. Once these routines are in place, choosing the right bedding can make managing accidents far less stressful.
Bedding Protection
Traditional waterproof mattress protectors and absorbent pads often require a lot of laundry after accidents, which can add to the stress of managing bedwetting. Thankfully, modern options have simplified this process.
PeelAways offers disposable, multi-layer waterproof fitted sheets with a patented peel-away design. Each sheet has 5–7 soft, absorbent layers (depending on the size). When an accident happens, you simply peel off the soiled layer to reveal a clean one underneath - no heavy mattress lifting, no late-night laundry sessions, and no risk of cross-contamination. These sheets not only protect the mattress but also give teens the ability to handle accidents on their own, discreetly and easily.
"These have saved my sanity! With 2 incontinent special needs teenagers... these have relieved a lot of stress. They hold a LOT of liquid and are easy to use and tear away. No more 15 loads of laundry and wet mattresses!"
– Jalene Stanger
"My 12-year-old son doesn't wake up sometimes and has accidents. These sheets are the perfect solution. They protect his mattress and they are discreet under his regular bed sheets. It has helped so much. When he has an accident he now can take care of it himself and put a new top sheet on his bed. No more scrubbing, no more smell, and no more embarrassment."
– Ronda
PeelAways are available in various sizes - Twin ($34.99), Full ($43.99), Queen ($47.99), and King ($53.99). Twin XL options come in both 5-layer and 7-layer designs. These practical solutions also work well for travel and social situations.
Travel and Sleepover Strategies
Bedwetting doesn’t have to stop your teen from enjoying sleepovers, camps, or trips. With a little preparation, they can confidently participate in these activities. Pack a discreet bag with portable bedding, extra pajamas, and a change of clothes for overnight stays. Portable bedwetting alarms can also help by alerting your teen during the night.
For added convenience, disposable options like PeelAways can be shipped directly to your destination, saving space in their luggage. Encourage your teen to limit fluids before bedtime and use the bathroom right before sleep. If appropriate, having an open conversation with a trusted adult - like a friend’s parent or a camp counselor - can help ensure any necessary accommodations are in place. This kind of support can make your teen feel included rather than isolated.
Treatment Options for Teen Bedwetting
When it comes to treating teen bedwetting, the best approach often depends on the root cause, the teen's willingness to engage in the process, and family preferences. Many healthcare professionals suggest starting with behavioral strategies before exploring medication. These methods aim to build on earlier interventions and offer meaningful relief.
Bedwetting Alarms
Bedwetting alarms are often the go-to option for teens who are motivated to address the issue. These devices feature a moisture sensor that’s placed in underwear or on the bed. If wetness is detected, the alarm emits a sound or vibration to wake the teen. Over time, this conditioning helps the brain associate bladder fullness with waking up before an accident happens. Consistent use is key - most teens see improvement within 2–3 months, but full success may take up to 3–6 months of nightly use. Research backs this up: one study found that combining alarms with an intensive behavioral plan led to a success rate exceeding 90% [9].
Medications for Bedwetting
For some teens, medication can play a role in managing bedwetting. Desmopressin is a commonly prescribed option. This synthetic hormone works by mimicking the body’s natural antidiuretic hormone, which reduces urine production during sleep. It’s effective in 20–30% of cases, although relapses are common once the medication is stopped [9]. Desmopressin comes as a nasal spray or tablet and should only be used under medical supervision due to potential side effects like low sodium levels.
In cases where bladder capacity is a concern, anticholinergic medications may be added to the treatment plan. These drugs help relax bladder muscles and increase its capacity, particularly for teens dealing with both daytime and nighttime control issues. As with desmopressin, these medications require careful monitoring by a healthcare provider.
Behavioral and Lifestyle Changes
Behavioral adjustments can make a big difference when applied consistently. One effective strategy is the double voiding method, which involves urinating twice before bed to ensure the bladder is empty. Setting a regular daytime schedule - encouraging bathroom visits every 2–3 hours - can also help train the bladder and reduce nighttime accidents.
Managing fluid intake is another critical step. Encourage proper hydration during the day but limit fluids 2–3 hours before bedtime. Addressing constipation is equally important, as impacted stool can press on the bladder and reduce its capacity. Teens experiencing pain or difficulty during bowel movements should prioritize resolving constipation by increasing fiber intake and establishing regular bathroom habits. Additionally, avoiding caffeine and sugary drinks in the evening can help prevent unnecessary bladder stimulation.
Emotional support is vital throughout this process. Bedwetting isn’t something teens can control, so shaming or punishing them only adds stress. Instead, involve them in small, manageable tasks like changing bedding to encourage responsibility without blame. Using a bedwetting calendar to track progress can also be encouraging, helping to identify patterns, celebrate milestones, and stay patient during setbacks.
sbb-itb-45288fe
Long-Term Success and Emotional Support
Building Emotional Resilience
Supporting your teen emotionally is just as important as addressing the physical aspects of bedwetting. This condition can take a toll on their self-esteem, often leading to feelings of embarrassment, social anxiety, and even isolation. Many teens may shy away from sleepovers, camps, or dating, fearing that an accident could reveal their condition. To help them build emotional resilience, start with how you approach the topic at home. Frame bedwetting as a medical issue that can be treated, and use neutral terms like "nocturnal enuresis" instead of words that might suggest laziness or immaturity.
It’s crucial to avoid blame, punishment, or visible frustration when accidents happen. These reactions can heighten stress and even worsen the situation. Instead, foster open communication. Ask your teen how bedwetting affects their life and listen attentively without brushing off their concerns. Involving them in decisions - like choosing a bedwetting alarm or selecting protective bedding - can give them a sense of control and dignity.
Privacy is another cornerstone of emotional support. Store supplies discreetly, keep bedroom doors closed during cleanup, and avoid discussing the issue in front of siblings or guests. Providing practical tools for independence can also make a big difference. For instance, products like PeelAways disposable waterproof sheets allow teens to clean up quickly and privately by peeling away a soiled layer to reveal a fresh one underneath. This kind of independence can help reduce feelings of shame and boost their confidence during treatment.
Tracking Progress and Handling Setbacks
Keeping a simple nighttime log can be a helpful way to track patterns and celebrate progress. Over time, this log might reveal triggers - for example, more frequent bedwetting during stressful school periods - or highlight gradual improvements that aren’t obvious on a daily basis.
Celebrate small victories. Whether it’s a string of dry nights, responding to an alarm earlier, or smaller wet patches, focusing on positive trends can be incredibly motivating. If you’re using a bedwetting alarm, stick with it for at least 6–12 weeks. Research shows that with consistent use, success rates range from 50% to 80%.
Setbacks are normal and should be expected. Illness, growth spurts, changes in routine, or increased stress can all cause temporary relapses. When these setbacks happen, work with your teen to identify potential causes and adjust the plan as needed. Remind them that a relapse doesn’t erase the progress they’ve made - it’s just another step in the process. Reviewing the log with a healthcare provider during follow-ups can also help refine strategies and keep things on track. These efforts teach teens to adapt and develop resilience as they grow.
Preparing for Adulthood
As teens approach adulthood, they’ll need to build on earlier strategies to manage their condition independently. For those heading to college or shared living situations, preparation is key. If bedwetting continues into the late teens, consulting a specialist - like an adolescent urologist or continence clinic - can provide further guidance and treatment options. Teens should have a clear understanding of their condition and which strategies work best for them, whether that involves alarms, medications, lifestyle changes, or protective bedding.
Planning ahead can ease anxiety about dorm life. Discreet solutions like quick-change bedding and waterproof mattress protectors can help avoid drawing attention. Storing supplies in opaque containers and scheduling bedding changes during private moments are simple ways to maintain discretion.
If a teen feels the need to disclose their condition, help them prepare a straightforward explanation, such as: "I have a sleep-related bladder condition that I’m managing with my doctor." For specific scenarios like overnight trips or exams, short-term medication options like desmopressin may also be worth discussing with a clinician. Teaching teens to manage their supplies, appointments, and treatment routines on their own is essential for building the confidence and independence they’ll need as they transition into adulthood.
Conclusion
Teen bedwetting is both common and manageable. It stems from a mix of physical and developmental factors - not from laziness or a flaw in character. Most teens grow out of it naturally, especially when families take a thoughtful approach that includes medical guidance, practical strategies, and emotional support. If bedwetting begins suddenly, continues into the mid-teens, or is accompanied by symptoms like pain or daytime accidents, it’s important to consult a primary care provider or pediatrician.
Managing bedwetting effectively requires a combination of approaches. Establishing consistent nighttime routines - like cutting back on fluids a couple of hours before bed, encouraging double voiding, and sticking to regular sleep schedules - creates a solid foundation. Bedwetting alarms, when used consistently over 8–12 weeks, are one of the most reliable long-term tools. For short-term relief in situations like sleepovers or camps, medications such as desmopressin can be helpful. According to the Mayo Clinic Health System, desmopressin has about a 30% success rate, but it works best when paired with behavioral changes. Protective bedding solutions, such as PeelAways, make cleanup easier and help reduce stress for both teens and parents.
Equally important is addressing the emotional side of bedwetting. Maintaining calm, private conversations about the issue and framing it as a medical condition - not a personal failing - can protect your teen’s self-esteem. Involve them in decision-making and celebrate small milestones, whether it’s fewer wet nights or quicker cleanups. This kind of support helps teens stay engaged in treatment and feel confident participating in activities like sleepovers or school trips.
Combining consistent routines with emotional support is key to long-term progress. Setbacks can happen, especially during times of illness or stress, so tracking progress in a diary can be helpful. Regular check-ins with healthcare providers - every 8–12 weeks - ensure steady improvement. If bedwetting continues into late adolescence, consulting a pediatric urologist or continence specialist may be necessary. With the right mix of medical care, practical solutions, and a supportive home environment, teens can maintain their confidence, fully engage in school and social activities, and gain the independence they need as they approach adulthood.
Related Articles
Check out these guides for practical solutions and tips on managing teen bedwetting.
Managing Bedwetting During Travel: Tips and Tools
Learn how to handle bedwetting while on the go with advice on creating discreet travel kits. These kits can include extra clothing, waterproof protection, and disposal supplies. The guide also highlights ways to maintain routines even when you're away from home. Diana L. Magda, a PeelAways customer, shared her experience:
I was going away to visit family and was worried about nighttime bladder leakage. I didn't want to ruin their bed and didn't want to lug a bunch of bulky under pads. I had these shipped directly to their home before I arrived. They were so easy to use, comfy, and never leaked!
- Diana L. Magda, Customer
How to Use Bedwetting Alarms Effectively
This guide walks you through setting up and using bedwetting alarms to train the brain to wake when the bladder is full. It includes realistic timelines for progress (typically 8–12 weeks), tips for helping deep sleepers, and additional strategies like double voiding and addressing constipation. It also explains when it might be time to consult a pediatrician.
PeelAways: The Best Bedding Solution for Bedwetting
Discover how multi-layer disposable sheets can make nightly cleanup quick and stress-free. These sheets, available in Twin, Twin XL, Full, Queen, and King sizes, feature 5–7 waterproof layers. Simply peel away the top layer to reveal a fresh one in under a minute - no heavy lifting or extra laundry required. They're a discreet and effective way to protect mattresses.
FAQs
What causes bedwetting in teenagers?
Teen bedwetting can stem from several causes, ranging from physical to emotional factors. Medical conditions like urinary tract infections or diabetes might be responsible, as well as hormonal imbalances that disrupt nighttime urine production. Sleep disorders, which make it difficult to wake up, and issues like reduced bladder capacity or overactive bladder muscles, can also contribute.
Stress and anxiety, particularly during significant life transitions, are frequent emotional triggers. Understanding the root cause is essential for determining the most effective way to address the issue.
How do bedwetting alarms work to help teens stop bedwetting?
Bedwetting alarms are tools designed to help teens become more aware of a full bladder while they sleep. These devices work by using a small sensor, typically placed in pajamas or bedding, to detect moisture. When it senses wetness, the alarm either sounds or vibrates, waking the individual so they can head to the bathroom.
With consistent use, this method can train the body to recognize the need to wake up before bedwetting happens. While results differ from person to person, many families find these alarms effective when approached with persistence and patience.
When is it time to see a doctor about teen bedwetting?
It's crucial to reach out to a doctor if bedwetting persists beyond age 7, begins suddenly after a period of dryness, or comes with other symptoms like pain, fever, or noticeable behavior changes. These signs might point to an underlying medical or emotional issue that requires attention.
Seeking medical advice early can help uncover the root cause and offer strategies to address the issue, ensuring your teen receives the care and support they need.
Related Blog Posts
Comments
0

SAVE MONEY & WATER
Professionals & Institutions save a fortune on labor/laundry.

SUPERIOR COMFORT
The first thing our customers notice is how soft our sheets are.
100% WATERPROOF
Each layer is 100% Waterproof, perfect for spills and accidents

SAVE TIME
Change the sheet in under 1 minute without stripping the bed.




Leave a comment