Ultimate Guide to Hand Hygiene in Care Settings

Hand hygiene is the simplest and most effective way to prevent infections in care settings like nursing homes and group homes. Proper hand hygiene can stop up to 50% of avoidable infections, saving lives and reducing costs. However, caregivers face challenges like time constraints, limited sink access, and misunderstandings about proper techniques.
Here’s what you need to know:
- Why It Matters: Infections like pneumonia, urinary tract infections, and C. difficile spread easily through unclean hands in group care settings.
- Key Techniques: Use soap and water for visibly dirty hands or during outbreaks. Alcohol-based hand rubs (ABHR) are effective for routine cleaning when hands aren’t visibly dirty.
- When to Wash: Follow the "Five Moments for Hand Hygiene" (e.g., before patient contact, after exposure to bodily fluids).
- Improving Compliance: Regular training, audits, and incentives can help caregivers follow hygiene protocols consistently.
- Additional Tools: Products like PeelAways disposable bedding reduce cross-contamination risks by simplifying soiled sheet changes.
Introduction to Just Clean Your Hands (Long Term Care)
Why Hand Hygiene Matters in Care Settings
Hand hygiene is the most effective way to prevent the spread of harmful germs and antibiotic resistance in healthcare environments [5]. Caregivers moving between residents or touching shared surfaces can unknowingly carry and spread microorganisms. If hands aren’t cleaned at the right times, infections can quickly take hold in group care settings, putting vulnerable residents at serious risk. This highlights the importance of understanding healthcare-associated infections (HAIs) and their impact.
Hand hygiene programs can prevent up to 50% of avoidable infections and deliver savings up to 16 times their cost [2]. For U.S. care facilities - many of which operate under strict budgets and regulatory oversight - this makes proper hand hygiene both a medical necessity and a smart financial decision.
What Are Healthcare-Associated Infections (HAIs)?
Healthcare-associated infections (HAIs) occur when patients develop infections while receiving care for unrelated conditions in settings like hospitals, nursing homes, or group homes. These infections are not present or incubating at the time of admission [3]. Often, HAIs spread through the hands of healthcare workers and caregivers, making hand hygiene a critical line of defense [2][3].
In the U.S., hundreds of thousands of patients develop HAIs each year, leading to significant illness, loss of life, and increased healthcare costs [3]. Common HAIs in care settings include:
- Respiratory infections like pneumonia
- Urinary tract infections (especially in residents with catheters)
- Skin and soft-tissue infections
- Gastrointestinal illnesses caused by norovirus or C. difficile
- Bloodstream infections
These infections often result from the transfer of pathogens through bodily fluids, contaminated surfaces, medical devices, or contact with an infected resident [3].
Proper hand hygiene breaks this chain of transmission by removing or killing harmful microorganisms before they can spread to another resident, a wound, or an invasive device [3]. The World Health Organization’s "Five Moments for Hand Hygiene" outlines when hand cleaning is most important: before touching a patient, before performing a clean or aseptic procedure, after exposure to bodily fluids, after patient contact, and after touching a patient’s surroundings [3]. Following these guidelines is essential for infection prevention.
Protecting High-Risk Populations
Certain groups in care settings are particularly vulnerable, including older adults, young children, and people with weakened immune systems - such as those undergoing chemotherapy, taking immunosuppressive drugs, or managing conditions like advanced diabetes, chronic kidney disease, or HIV [3]. For these individuals, even small lapses in hand hygiene can have serious consequences.
Older adults face unique risks due to chronic illnesses, reduced mobility, and the use of medical devices like catheters or feeding tubes [3]. These factors increase their susceptibility to infections when microorganisms are transferred via caregivers’ hands. Many elderly residents also require help with feeding or oral care, which can introduce pathogens into their airways or digestive systems. For dementia patients, consistent hand hygiene is especially critical to prevent cross-contamination.
Children and individuals with special needs are prone to rapid spread of respiratory viruses like RSV and influenza, as well as gastrointestinal infections from pathogens like norovirus [2][4]. These groups often need close physical assistance with daily activities, such as feeding or toileting, which creates frequent opportunities for caregivers’ hands to come into contact with saliva, nasal secretions, or stool [4]. For children who mouth objects or frequently touch surfaces, clean hands act as a protective barrier against harmful microbes.
Residents with weakened immune systems or complex medical conditions are at an even higher risk. Infections that may cause mild symptoms in others can lead to severe complications like sepsis, pneumonia, or bloodstream infections in these individuals [3]. Medical devices like central lines, dialysis catheters, or tracheostomies provide direct entry points for germs, making hand hygiene before handling these devices absolutely essential [2][3].
Failing to maintain proper hand hygiene can result in outbreaks, increased hospitalizations, and even death, especially for frail or immunocompromised individuals [3]. Beyond the human toll, poor hygiene can lead to higher costs for facilities due to additional treatments, protective equipment, and staffing needs. It can also attract regulatory scrutiny and damage a facility’s reputation if infection rates reveal lapses in basic prevention practices [2][3][5].
Hand Hygiene Techniques and Best Practices
WHO 6-Step Hand Hygiene Technique for Healthcare Workers
When it comes to keeping your hands clean, the method you choose depends on the situation. Use soap and water for visible dirt or contamination, while alcohol-based hand rubs (ABHR) are ideal for routine cleaning when hands aren't visibly dirty. Both approaches are essential in stopping the spread of germs, but they work in different ways. For high-frequency situations where time is limited, ABHR offers a quick and effective solution.
How to Wash Hands with Soap and Water
Start by wetting your hands with warm water and applying liquid soap - about the size of a nickel or quarter [4]. Scrub every surface of your hands for at least 15–20 seconds [4], ensuring thorough cleaning.
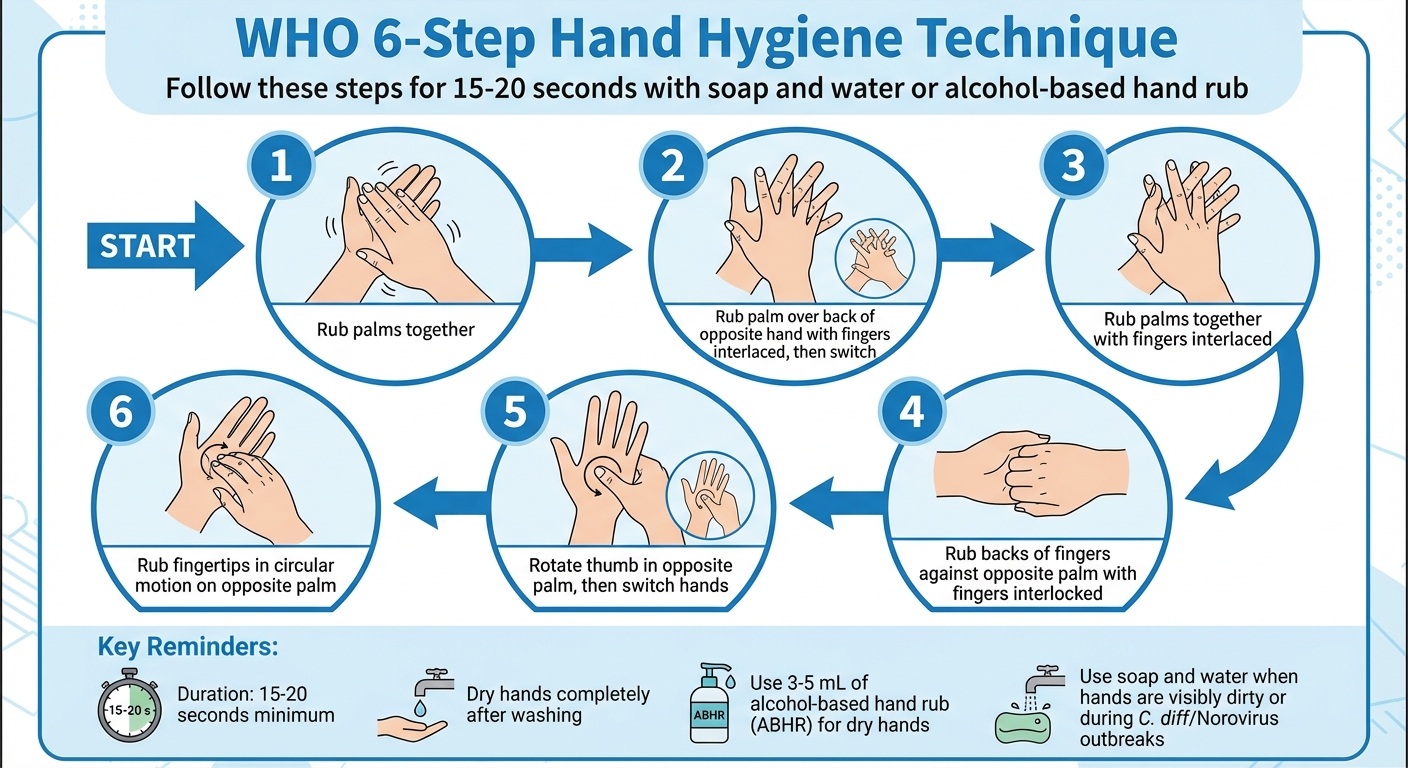
The World Health Organization (WHO) recommends a 6-step handwashing technique to cover all areas [3]:
- Press your palms together and rub.
- Place your right palm over the back of your left hand, interlacing your fingers, and repeat with the other hand.
- Rub your palms together with fingers interlaced.
- Press the backs of your fingers against the opposite palm, interlocking your fingers.
- Rotate your thumb in the opposite palm, then switch hands.
- Rub your fingertips in a circular motion on the opposite palm.
After scrubbing, rinse your hands well under running water and dry them completely with a single-use towel. Drying is crucial - damp hands are more likely to transfer germs.
Soap and water are the go-to choice when your hands are visibly dirty, contaminated with body fluids, after restroom use, before eating, or after touching surfaces in a patient’s area. This method physically removes dirt, oils, and certain pathogens that alcohol-based products can't tackle.
When and How to Use Alcohol-Based Hand Rubs
For situations where your hands aren’t visibly dirty, ABHR containing 60–80% alcohol is highly effective [1]. It works faster than soap and water, is gentler on the skin, and is perfect for quick transitions.
To use ABHR properly, apply 3–5 mL (enough to cover all hand surfaces) to your palm. Rub your hands vigorously, following the same 6-step technique as with soap and water. Make sure to cover every part of your hands, including palms, backs, between fingers, thumbs, fingertips, and wrists. Continue rubbing until your hands are completely dry - this usually takes about 20 seconds, allowing the alcohol to do its job.
Most ABHR products include moisturizers like glycerol to combat dryness, but frequent use can lead to residue buildup. To avoid this, wash your hands with soap and water occasionally to remove any residue.
Remember, ABHR isn’t suitable for every situation. It doesn’t work against spore-forming infections like Clostridioides difficile (C. diff) or Norovirus. In these cases, soap and water are the only reliable option [1].
Hand Hygiene During C. difficile and Other Outbreaks
During outbreaks of tough-to-kill pathogens like C. diff or Norovirus, hand hygiene requires extra care. ABHR is ineffective against these spore-based infections [1], so switch exclusively to soap and water.
When dealing with outbreaks, wash your hands after every patient interaction, after touching surfaces, after removing gloves, and after using the restroom. Pay close attention to areas where spores can hide, like under your nails. In these situations, even if ABHR has been effective in the past, it’s critical to adapt your approach immediately to prevent further spread.
The same rule applies to other spore-forming organisms like Bacillus anthracis. When in doubt, always choose soap and water - it’s the safest way to protect yourself and others during outbreaks.
How to Improve Hand Hygiene Compliance
Hand hygiene compliance often struggles to exceed 40–50%, largely due to challenges like time constraints, inconveniently placed dispensers, skin irritation, forgetfulness, and a lack of emphasis on safety in the workplace. However, structured strategies can significantly boost compliance rates and help reduce infections [2].
The World Health Organization's Multimodal Hand Hygiene Improvement Strategy offers a practical framework. This approach emphasizes making hand hygiene products easily accessible, providing continuous training and education, monitoring compliance with regular feedback, using workplace reminders, and cultivating a strong safety culture [2]. Below, we’ll explore how training, audits, and incentives can elevate hand hygiene practices.
Staff Training and Education Programs
Training plays a key role in overcoming the barriers to hand hygiene compliance. For it to be effective, training should be recurring and use a mix of approaches - short classroom or online modules, practical demonstrations, and scenarios tailored to specific roles [2]. For instance, care assistants might focus on hygiene during toileting, feeding, and bed-making, while nurses could concentrate on tasks like medication administration and wound care.
Brief, five- to ten-minute micro-training sessions during shift huddles help reinforce these lessons. Adding competency checks and U.S.-specific case studies of healthcare-associated infections keeps the topic relevant and engaging. When caregivers see the direct link between proper hand hygiene and protecting both residents and themselves, they’re more likely to follow through [2].
Monitoring Compliance Through Audits and Observation
Regular audits are essential for turning good intentions into consistent actions. Facilities can assign trained observers to conduct short, periodic audits during routine care. Using standardized tools, such as WHO’s hand hygiene observation forms, helps track whether opportunities for hand hygiene are utilized or missed. Presenting this data as unit-level trends and framing audits as safety tools - not punitive measures - encourages participation.
Observers can also provide immediate, respectful coaching. For example, they might suggest attaching a sanitizer holder to a badge for easier access during room-to-room care. Involving frontline staff in creating the audit process builds trust and ownership. Additionally, tracking key metrics like the percentage of correctly completed hand hygiene opportunities, product usage (e.g., alcohol-based sanitizer per patient-day), and infection rates provides actionable insights. Sharing this data through visual dashboards or monthly scorecards can motivate teams to improve [2].
Using Incentives and Feedback to Encourage Compliance
Positive reinforcement tends to be more effective than punishment for encouraging compliance. Simple strategies like monthly competitions or unit-level rewards - think breakfast treats or small gift cards - can make a big difference in motivating staff and fostering team pride.
Providing timely and specific feedback is equally important. Regular unit meetings can review anonymized data trends, celebrate progress, and address any challenges. One-on-one coaching should focus on practical workflow improvements, avoiding blame, and reinforcing the role of hand hygiene in overall patient safety [2].
Hand hygiene compliance can also be linked with other infection prevention practices. For example, proper hand hygiene before and after handling disposable, multi-layer sheets can help reduce cross-contamination. When these practices are viewed as interconnected parts of a broader safety culture instead of isolated tasks, they become second nature [2].
sbb-itb-45288fe
Nail Care and Proper Glove Use
Hand hygiene goes beyond just washing your hands - what’s on your hands matters, too. Proper nail care and glove use are essential in reducing the spread of infections in healthcare settings. Ignoring either can undo even the most careful handwashing efforts.
Nail Hygiene Standards
Keeping nails short and clean is a must. Trim them straight across weekly, ensuring they don’t extend more than ¼ inch (6 mm) beyond the fingertip. Smooth out any rough edges with a file to prevent snags. Short nails are easier to clean and less likely to trap bacteria or cause accidental scratches during care. For staff with direct patient contact, artificial nails, gels, acrylics, and other nail enhancements are typically off-limits since they can harbor significantly more bacteria. Chipped nail polish is also a concern - it can trap microbes - so many facilities require either unpolished nails or polish that’s promptly removed if it begins to chip.
Daily nail care is just as important as trimming. Scrubbing under the nails during each handwashing session (about ten seconds with soap and water) can remove nearly all gram-negative bacteria. Avoid habits like biting nails or picking at cuticles, as these can create small skin breaks that increase infection risks. Using approved moisturizers helps prevent dryness, which can also harbor bacteria. Good nail hygiene lays the foundation for effective glove use in infection prevention.
When and How to Use Gloves Correctly
Once your nails are clean and well-maintained, the next step is knowing how to use gloves properly to maintain a protective barrier. Gloves should be worn whenever there’s a chance of coming into contact with blood, bodily fluids, mucous membranes, non-intact skin, or contaminated surfaces. For example, gloves are essential during tasks like perineal care, wound care, or handling soiled linens. However, for brief, dry contact with intact skin - such as assisting a resident to walk or taking blood pressure - gloves aren’t usually necessary.
It’s important to remember that gloves don’t replace hand hygiene. Always clean your hands before putting on gloves and immediately after removing them.
Here’s how to safely remove disposable gloves:
- Pinch the outside of one glove at the wrist and peel it off, turning it inside out.
- Hold the removed glove in your gloved hand. Slide your fingers under the wrist of the remaining glove without touching your skin, then peel it off inside out.
- Dispose of the gloves right away and wash your hands.
Never reuse disposable gloves, and avoid touching clean surfaces with contaminated gloves. Always change gloves between residents and tasks. During outbreaks of pathogens like C. difficile or Norovirus, change gloves immediately after contact with feces or vomit and wash hands with soap and water, as alcohol-based hand rubs may not be effective against these organisms.
By combining proper nail care, glove use, and routine hand hygiene, the risk of infection can be significantly reduced. Using products like PeelAways can further help minimize contamination in bedding and other surfaces.
PeelAways: Reducing Cross-Contamination in Bedding
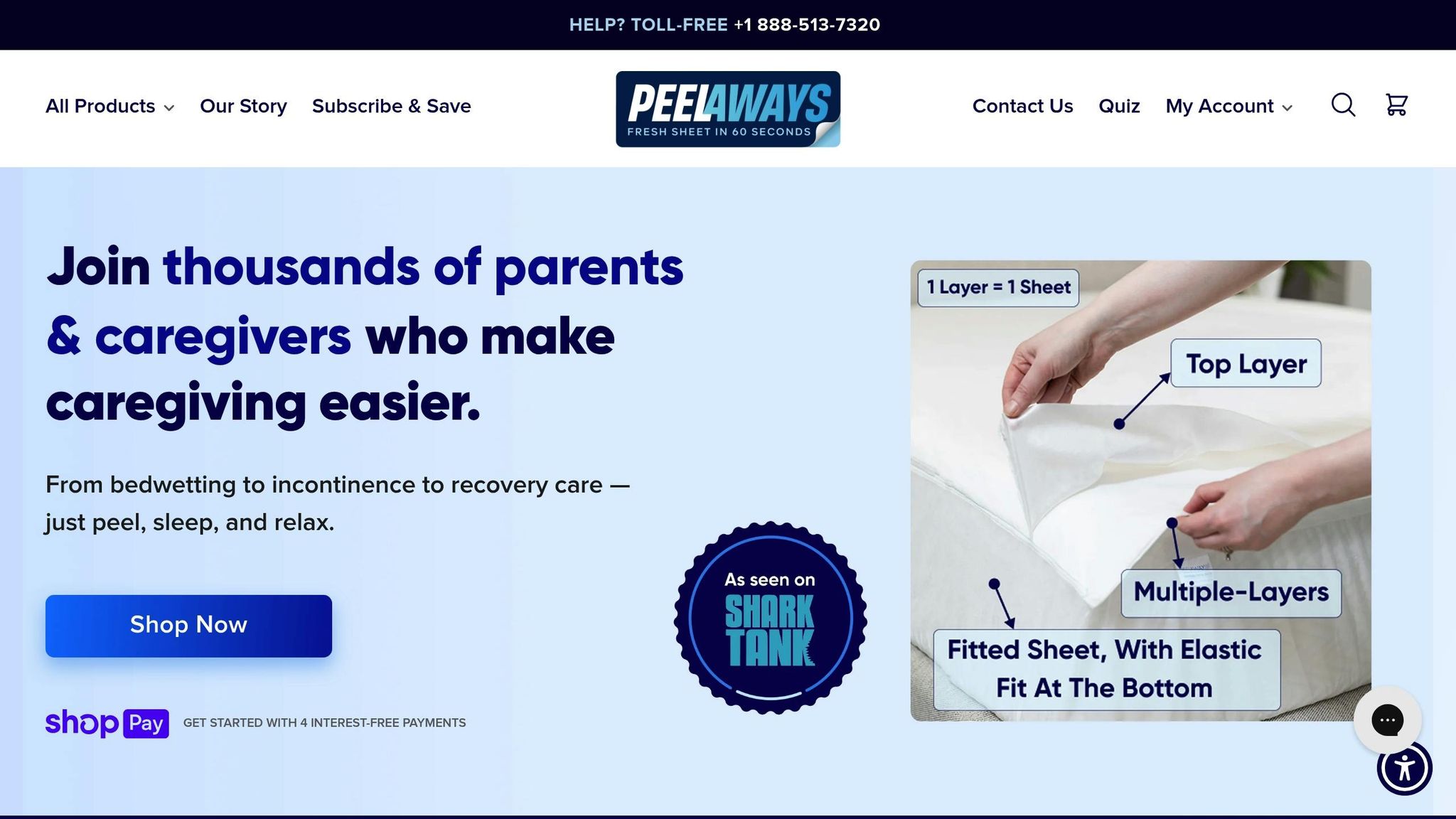
Even with proper handwashing, soiled bedding can still spread harmful pathogens like C. difficile and MRSA. Each bedding change introduces the risk of cross-contamination. PeelAways disposable sheets take a different route, cutting out many of these high-risk touchpoints. Here’s a closer look at how their multi-layer design helps minimize the spread of germs.
How PeelAways Multi-Layer Sheets Work
PeelAways fitted sheets come with 5–7 absorbent, waterproof layers (7 layers for Cot and Twin XL; 5 layers for Twin, Full, Queen, and King). These layers are designed to block fluids like urine, blood, and wound drainage from soaking through to the mattress or the layers below. When a layer gets soiled, you simply peel it off, roll it inward, and discard it - leaving a fresh, clean sheet underneath in seconds. No need to lift the mattress, strip the bed, or deal with laundry. Unlike underpads that can bunch up or slide around, PeelAways stay securely in place like a standard fitted sheet.
Hygiene Benefits for Caregivers and Patients
By allowing immediate disposal of soiled layers, PeelAways reduce the need to touch contaminated bedding. Instead of handling wet, germ-laden linens - which the CDC identifies as potential pathogen reservoirs - caregivers can peel off the top layer and discard it before washing their hands. Jalene Stanger, a caregiver for two incontinent special needs teenagers, shared her experience:
"They absorb significant liquid, simplify changes, and eliminate excessive laundry."
For patients, the benefits are just as clear. PeelAways provide a consistently clean, dry surface, helping to prevent skin irritation and infection - especially important for those with weakened immune systems. The breathable, waterproof design keeps the bed cool and comfortable while protecting against fluids. Ronda, a mother, explained how PeelAways transformed her 12-year-old son’s life:
"When he has an accident he now can take care of it himself and put a new top sheet on his bed. No more scrubbing, no more smell, and no more embarrassment."
With over 12,000 satisfied customers and an average 4.8-star rating [6], caregivers frequently highlight how PeelAways make bedding changes easier and improve hygiene.
Uses in Elder Care, Special Needs, and Medical Recovery
PeelAways aren’t just for home use - they’re a practical solution in many care environments. In elder care facilities, for instance, they simplify overnight incontinence management. After an incident, caregivers can remove the soiled layer without repositioning the resident or lifting the mattress, then follow CDC hand hygiene protocols. This process reduces the risk of spreading germs, which is common when handling heavily soiled reusable linens.
Available in a range of sizes - including Crib-A-Peel for toddlers, Cot, Twin XL (7 layers), and standard Twin, Full, Queen, and King - PeelAways fit seamlessly into various settings. During critical times, such as acute illnesses or C. difficile outbreaks, they provide an immediate clean barrier. This aligns with WHO recommendations, which suggest that proper bedding practices can cut healthcare-associated infections by up to 50% [2].
Key Takeaways
Maintaining proper hand hygiene is one of the simplest and most effective ways to prevent healthcare-associated infections in care environments. Washing hands with soap and water for 15–20 seconds effectively removes nearly all transient bacteria. In situations where hands aren’t visibly dirty, alcohol-based hand rubs (containing 60–80% alcohol) offer a faster alternative, especially in settings where frequent contact occurs.
Effective techniques are just part of the equation - strong compliance strategies are equally important. Following the WHO’s "Five Moments for Hand Hygiene" helps target key points where bacteria transmission is most likely. During specific outbreaks, like those caused by Clostridioides difficile, using soap and water is critical since alcohol-based sanitizers are less effective in such cases.
Compliance improves significantly when healthcare facilities adopt a multimodal approach. This includes staff training, regular audits, feedback, and even incentives. The WHO’s multimodal strategy has proven to be highly cost-effective, delivering savings up to 16 times the investment while preventing up to 50% of avoidable infections [2].
Reducing contamination risks also involves limiting touchpoints. For example, PeelAways multi-layer sheets provide a practical solution for soiled bedding. These sheets, which come with 5–7 waterproof layers depending on size, allow caregivers to simply peel off the top layer to reveal a clean sheet underneath. They’re available in various sizes, from Crib-A-Peel for toddlers to King sizes, and are especially useful in maintaining a clean environment. When combined with rigorous hand hygiene practices, these sheets further lower the risk of contamination.
A comprehensive approach that includes proper hand hygiene, nail care, correct glove use, and smart bedding solutions creates a strong barrier against infection transmission. This protects both caregivers and the vulnerable individuals under their care.
Related Articles
Check out these articles for practical advice on hygiene, infection prevention, and making caregiving easier with PeelAways. Each piece expands on key hand hygiene practices and PeelAways' innovative bedding solutions to support a thorough approach to infection control.
5 Ways PeelAways Simplifies Caregiving - Learn how PeelAways' multi-layer disposable sheets cut down on handling soiled linens and limit exposure to body fluids, improving infection control in care facilities across the U.S.
How to Prevent Cross-Contamination in Group Care - Follow actionable steps that pair WHO's "Five Moments for Hand Hygiene" with PeelAways' easy-to-use bedding to reduce cross-contamination in shared care environments.
Top Hygiene Tips for Elderly Caregivers - Get a daily hygiene checklist designed for caregivers. This guide combines essential hand hygiene practices with PeelAways bedding to help protect older adults from harmful contaminants.
FAQs
What are the 'Five Moments for Hand Hygiene' and why do they matter in care settings?
The 'Five Moments for Hand Hygiene' emphasize key instances when healthcare workers should clean their hands to help stop the spread of infections. These moments include:
- Before coming into contact with a patient
- Before carrying out clean or aseptic procedures
- After being exposed to body fluids
- After physical contact with a patient
- After touching objects or surfaces in a patient’s surroundings
By adhering to these guidelines, healthcare providers can greatly lower the chances of cross-contamination, safeguard patient well-being, and promote a safer care environment.
Are alcohol-based hand rubs as effective as washing with soap and water?
When your hands aren't visibly dirty or greasy, alcohol-based hand rubs do a great job of killing most germs, including bacteria and viruses. However, soap and water take the lead when it comes to removing dirt, organic matter, and stubborn pathogens like Clostridioides difficile spores. For the best hand hygiene, stick to soap and water for cleaning visibly dirty hands, and reach for alcohol-based rubs for a quick sanitize when your hands appear clean.
How can caregivers improve hand hygiene compliance in care settings?
Improving hand hygiene compliance in care settings begins with educating staff on proper techniques and emphasizing its importance for patient safety. Regular training sessions, paired with open communication, help ensure these practices become second nature.
Using visible reminders like posters or signs near sinks and hand sanitizer stations can keep hygiene at the forefront. Additionally, making hand hygiene stations with alcohol-based sanitizers easily accessible encourages frequent use by removing barriers to convenience.
Fostering a culture of accountability plays a crucial role as well. Leadership should actively support safety initiatives, monitor adherence, and provide constructive feedback to uphold high standards. Even simple actions, like cleaning hands before and after every patient interaction, can significantly reduce the risk of infections.
Related Blog Posts
Comments
0

SAVE MONEY & WATER
Professionals & Institutions save a fortune on labor/laundry.

SUPERIOR COMFORT
The first thing our customers notice is how soft our sheets are.
100% WATERPROOF
Each layer is 100% Waterproof, perfect for spills and accidents

SAVE TIME
Change the sheet in under 1 minute without stripping the bed.




Leave a comment