Ultimate Guide to Laundry Hygiene in Care Facilities

Laundry hygiene in care facilities is a critical aspect of infection control. Contaminated linens can spread harmful bacteria, viruses, and ectoparasites, posing risks to residents and staff. Proper handling, washing, and storage practices are essential to prevent cross-contamination and ensure safety. Here's a quick overview:
- Key Risks: Contaminated textiles can spread infections, especially among residents with weakened immune systems or open wounds.
- Challenges: High laundry volumes, labor shortages, outdated facilities, and regulatory compliance create hurdles.
- Best Practices:
- Modern Solutions: Products like PeelAways disposable sheets reduce laundry loads and contamination risks, saving time and resources.
This guide outlines step-by-step protocols to improve laundry hygiene while protecting residents and staff from infection risks.
Infection Control Basics for Healthcare Laundry Services: Part 1
How to Sort and Handle Soiled Linens
Managing soiled linens properly is a critical step in infection control within any care facility. These linens often carry bodily fluids like blood, stool, urine, or vomit, which can harbor harmful bacteria and viruses if not handled correctly[3]. The way staff collect, sort, and transport these items plays a key role in maintaining a safe environment.
Safe Handling Steps
When dealing with soiled linens, staff should always wear appropriate personal protective equipment (PPE), including gloves, gowns, and masks. According to CDC guidelines, high-quality PPE should be easily accessible at all laundry handling points[2][4]. Gloves used for sorting should also provide adequate protection against potential sharps[3].
Linens must be bagged or contained right where they’re collected - inside the resident care area, not in hallways or entryways - to minimize the spread of contaminants[5]. Use leak-proof, labeled bags or carts for this purpose, and avoid carrying bags against your body. To further reduce contact, no-touch hampers are a great option.
For transportation, use covered carts with leak-proof designs and secure lids to prevent spills and limit airborne exposure[7]. If linens are wet and could soak through cloth bags, opt for leak-resistant containers instead[3].
Sorting Methods
Sorting soiled linens by type and level of contamination helps optimize washing processes[7]. Common categories include:
- Heavily soiled items: Linens with significant bodily fluids.
- Lightly soiled items: Routine bed linens and towels.
- Specialty items: Personal clothing or incontinence-related linens.
OSHA guidelines emphasize separating infectious materials, like blood-soaked linens or items exposed to hazardous chemicals, from noninfectious ones to prevent exposure incidents[2]. Facilities often use color-coded bags or biohazard symbols - red bags are a popular choice for identifying items needing special handling[3].
Before sorting, staff should inspect each item carefully. Hard objects, such as syringes, needles, or personal belongings, must be removed to avoid damaging equipment or contaminating the washing process[7]. Solids like feces or vomit should also be removed before washing to protect commercial laundry machines[3].
How to Prevent Cross-Contamination
To prevent the spread of pathogens, avoid shaking soiled linens, as this can release contaminants into the air[5]. Sorting or pre-rinsing linens should never occur in resident care areas, hallways, or other open spaces. These tasks should be confined to designated laundry rooms.
Laundry rooms should be well-organized, with separate areas for soiled and clean linens. Physical barriers, such as walls or partitions, should divide these zones, and the soiled area should maintain negative air pressure to contain airborne contaminants[7]. Handwashing stations must be conveniently located, and clean linens should be stored in protected spaces, far from soiled items.
Regular training for staff is essential to ensure proper sorting and handling of soiled linens. Providing routine refresher courses helps reinforce these practices and ensures compliance with OSHA and CDC standards[2][4].
Washing and Sanitization Steps
Once soiled linens are properly sorted and contained, the washing process becomes a crucial step in eliminating pathogens and ensuring resident safety. Effective disinfection depends on the right combination of water temperature, detergents, and washing cycles.
Recommended Washing Cycles
After sorting, the washing process should follow a structured three-phase approach: pre-wash, main wash, and rinse cycle. This method ensures thorough cleaning and helps maintain infection control standards.
- Pre-wash: This step, performed at around 60°F (15°C), removes visible contaminants like blood, feces, or vomit. By addressing these substances early, the pre-wash prevents them from setting during the high-temperature main wash.
- Main wash: Linens are disinfected using hospital-grade detergents that meet COSHH standards. Chemical disinfectants used in this phase must be compatible with the detergents and also comply with COSHH requirements. Commercial laundry machines are ideal for maintaining consistent results, precise temperature control, and compliance with HTM 01-04 and OSHA standards.
- Rinse cycle: This final phase removes any residual chemicals or detergent buildup, which helps prevent skin irritation and ensures that no harmful residues remain on the linens.
Water Temperature and Detergent Guidelines
Temperature and detergent selection are critical for effective disinfection. According to the Centers for Disease Control and Prevention (CDC), linens should be washed at a minimum of 160°F (71°C) for at least 25 minutes to achieve proper thermal disinfection in healthcare settings.
Research shows that washing at 160°F (71°C) for 25 minutes reduces bacteria by 99.9%. Lower temperatures are far less effective, making precise temperature control a non-negotiable part of laundry operations in care facilities.
"Washing linens at higher temperatures significantly reduces the risk of infection transmission in healthcare settings." - Dr. Emily Johnson, Infection Control Specialist, CDC [1]
For heat-sensitive items, chemical disinfection at lower temperatures is an option. However, these methods require careful monitoring to ensure effectiveness. Disinfectants must be used as directed by the manufacturer, and staff should document their use thoroughly.
To maintain compliance and quality assurance, machines should be calibrated regularly, and temperature logs should be kept. Detailed records of washing cycles, achieved temperatures, and chemicals used are essential for passing inspections.
Infection Control During Washing
Maintaining infection control during the washing process is just as important as the washing itself. For heavily soiled linens, a double-wash is often recommended, particularly for items contaminated with blood, multiple bodily fluids, or materials from residents with infectious conditions.
Chemical disinfectants should be stored correctly and handled with proper personal protective equipment (PPE). Timing is critical - disinfectants must be added at the right point in the cycle to maximize their effectiveness.
To prevent cross-contamination, clean and soiled linens must be kept separate at all times. Strict hand hygiene is essential, with handwashing stations conveniently located in laundry areas for use before and after handling linens.
Regular maintenance of laundry equipment is another key aspect of infection control. Machines should be cleaned and disinfected after each use, or at least daily in high-volume settings. Maintenance tasks like calibration checks, filter cleaning, and inspections for lint or other contaminants should also be part of the routine.
Ongoing staff training plays a vital role in ensuring these protocols are consistently followed. Training should cover PPE use, chemical handling, emergency procedures, and regulatory guidelines, with refresher courses provided every six months.
sbb-itb-45288fe
Drying, Storage, and Transport of Clean Linens
Handling clean linens properly is crucial for maintaining hygiene and preventing healthcare-associated infections. The final steps - drying, storing, and transporting - play a pivotal role in ensuring linens remain uncontaminated.
Proper Drying Methods
Drying linens thoroughly is essential to prevent the moisture that encourages bacteria and mold. Healthcare facilities should use commercial-grade dryers that meet CDC recommendations: maintaining a temperature of 160°F (71°C) for at least 25 minutes [8][6]. This process ensures effective elimination of harmful microorganisms. Heat-sensitive items, however, should be dried at lower temperatures to avoid damage.
"The importance of proper drying cannot be overstated; it is a key factor in maintaining hygiene standards in care facilities."
– Dr. Emily Johnson, Infection Control Specialist
Dryers must be cleaned and disinfected regularly, following manufacturer guidelines, to avoid buildup of lint or contaminants. Once linens are dry, they should be promptly removed to prevent recontamination. This step ensures linens are ready for safe storage.
Clean Storage Practices
After drying, linens must be stored in areas specifically designated for clean items, separate from soiled laundry zones. Physical separation - such as using dedicated rooms or clearly marked sections - is critical to prevent cross-contamination. To further safeguard hygiene, the clean side of laundry facilities should maintain positive air pressure relative to soiled areas, reducing the risk of airborne contaminants [9].
Storage spaces should feature nonporous shelving made of materials like plastic or metal, which are easy to clean and disinfect. These areas must remain free from dust, pests, moisture, personal belongings, food, or cleaning chemicals. To protect linens, fold and seal them immediately after drying. A first-in, first-out (FIFO) system helps ensure older linens are used before newer stock, maintaining freshness and reducing waste. Regular inspections and cleaning of storage areas, along with limiting access to trained personnel, further support hygiene standards.
Once storage is secured, attention must shift to the safe transport of linens.
Safe Transport of Clean Linens
The separation of clean and soiled items must be upheld during transport. Clean linens should be moved using dedicated, covered carts that are never used for soiled items. A color-coded or clearly labeled system for transport equipment can help prevent cross-contamination.
Transport routes should avoid areas with soiled items, waste, or heavy foot traffic. Staff handling clean linens must follow strict hand hygiene protocols and wear clean uniforms. Linens should never be placed on floors or other potentially contaminated surfaces. Additionally, transport containers should be inspected regularly for cleanliness, and staff should receive proper training in handling practices. These measures significantly reduce the risk of contamination and ensure clean linens remain safe for use.
Disposable Bedding Solutions: PeelAways Multi-Layer Sheets
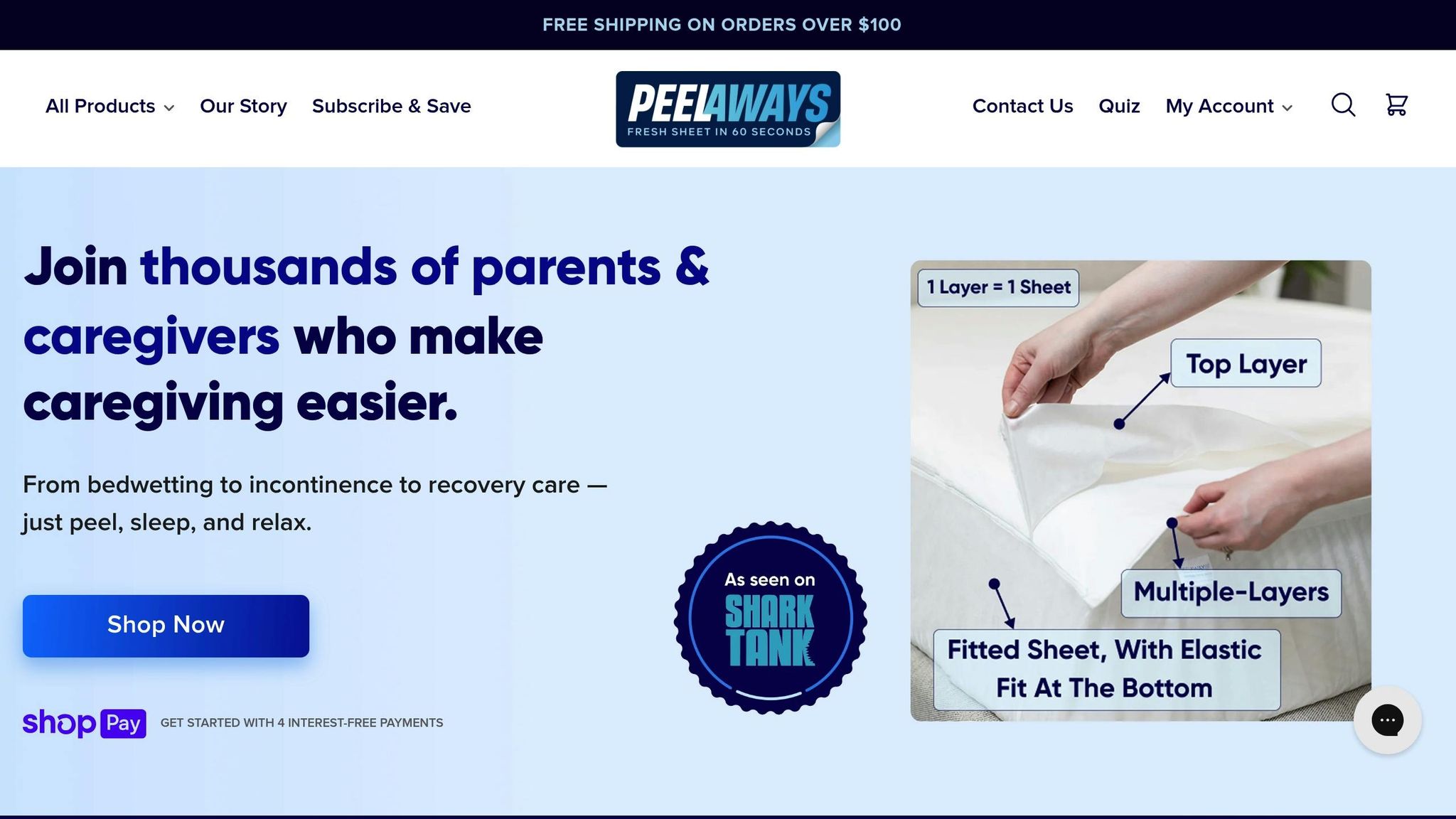
Laundry routines in care facilities can be time-consuming and costly. PeelAways disposable, multi-layer sheets offer a practical alternative, simplifying hygiene management while helping to reduce contamination risks. These sheets are designed to ease infection control and streamline bedding changes, making them a valuable addition to care settings.
What Are PeelAways?
PeelAways are disposable, waterproof bed sheets with a patented multi-layer design, offering 5 to 7 absorbent layers depending on the size. When a layer becomes soiled, caregivers can simply peel it off to reveal a fresh, clean sheet underneath. This eliminates the need to lift mattresses or handle traditional linens, significantly reducing the potential for cross-contamination.
These sheets function like fitted sheets, creating a protective barrier over the mattress. Each layer is engineered to absorb and contain liquids without leaking through to the next, keeping the mattress clean and maintaining patient comfort. The waterproof material blocks fluids while allowing air circulation, ensuring a hygienic and comfortable sleeping environment.
PeelAways are available in sizes ranging from toddler to King, with prices between $30.99 and $53.99.
Benefits for Care Facilities
One of the standout features of PeelAways is their ability to minimize cross-contamination. By allowing immediate removal of soiled layers, staff can avoid handling contaminated linens, reducing exposure to pathogens. This aligns with guidelines from the CDC and OSHA aimed at limiting contact with infectious materials [2][4].
Traditional laundry operations in care facilities can consume up to 20% of operational budgets and pose a significant risk for spreading infections [3][9]. PeelAways eliminate the need for frequent laundering, cutting down on water and detergent use, as well as the time spent sorting, washing, and storing linens.
"These have saved my sanity! With 2 incontinent special needs teenagers... these have relieved a lot of stress." - Jalene Stanger, PeelAways User
The time savings are also noteworthy. Changing a PeelAways sheet takes less than a minute, offering a stark contrast to traditional bedding changes that involve stripping the bed and washing linens. This efficiency is especially valuable in care facilities facing staff shortages or high turnover rates.
Research shows that proper laundry hygiene can cut infection rates by up to 30% in long-term care settings [3][5]. PeelAways contribute to these efforts by offering a disposable system that supports infection control and reduces the risks of healthcare-associated infections [2][4][9].
How to Use PeelAways in Care Settings
PeelAways are an effective complement to existing laundry protocols, particularly in environments where hygiene is critical but traditional laundering can be challenging. They are ideal for elder care, incontinence management, special needs care, and medical recovery settings. In long-term care facilities, where accidents are frequent, PeelAways allow for quick bedding changes without disturbing residents or exposing staff to bodily fluids.
The product's performance is backed by user experiences:
"After cleanup, I peeled away the top layer and found no leakage or odor." - Stephanie Jackson, PeelAways User
For pediatric care during potty training or in post-surgical recovery, the 100% waterproof design ensures reliable protection while remaining gentle on sensitive skin. Free from harsh chemicals, these sheets are safe for individuals with allergies or skin conditions, making them a trusted choice in care settings.
To maximize the benefits of PeelAways, staff should be trained in proper peeling techniques and disposal methods in line with local waste management regulations. The multi-layer design allows each set to last through several uses, reducing disruptions and maintaining hygiene standards.
Facilities that have adopted PeelAways report 50% reductions in laundry loads, leading to savings in labor, utilities, and equipment maintenance [9][10]. With an average rating of 4.8 out of 5 from over 12,000 users, PeelAways have proven to be a reliable solution for improving infection control and operational efficiency across various care environments.
Summary: Key Points for Laundry Hygiene
Maintaining proper laundry hygiene requires a step-by-step approach that ensures the safety of both residents and staff while keeping operations running smoothly.
Why a Comprehensive System Is Essential
An effective system prevents cross-contamination by strictly separating clean and soiled linens and following precise handling procedures. Physical barriers between these areas, along with dedicated transportation tools, provide extra layers of defense against the spread of harmful pathogens.
Regularly cleaning and maintaining laundry equipment helps avoid contamination caused by the machines themselves. Clear, documented protocols ensure staff adhere to regulatory standards, creating a solid framework for introducing newer, more efficient solutions.
Simplifying Laundry with Modern Solutions
Modern disposable bedding offers a practical way to streamline laundry processes. Traditional laundry setups often struggle with labor shortages and infection control challenges. Products like PeelAways make bedding changes faster - taking just about a minute - and eliminate the need for traditional washing.
Because these products are disposable, they align with infection control best practices by reducing contact with contaminated linens. This makes them particularly effective in environments where infection prevention is critical.
Steps for Improving Care Facility Practices
To enhance your laundry hygiene program, start by reviewing and updating protocols to align with OSHA and CDC guidelines. Create distinct zones for clean and soiled linens, and consider adopting disposable bedding in areas where infection risks are higher.
Ensure laundry areas are physically divided, with negative air pressure maintained in soiled zones. For facilities dealing with frequent accidents or high-risk situations, begin implementing changes in high-turnover areas or for residents with incontinence to evaluate the impact.
Track infection rates and compliance levels to measure progress and identify opportunities for further improvements in your laundry hygiene practices.
FAQs
What are the benefits of using Peelaways disposable sheets in care facilities, and how do they help prevent infections?
Peelaways disposable sheets are built with a multi-layered, waterproof design, making them a practical option for care facilities. Each sheet includes 5 to 7 soft, absorbent layers that can be peeled away effortlessly when soiled, instantly revealing a fresh, clean layer. This eliminates the need for washing and reduces physical tasks like lifting mattresses.
By minimizing the handling of soiled linens, Peelaways help decrease the chances of cross-contamination and infection spread. They offer a time-saving, cost-effective alternative to traditional bedding, providing caregivers and staff with a more hygienic and convenient solution.
What steps should care facilities take to meet CDC and OSHA guidelines for handling and washing soiled linens?
Care facilities can stay aligned with CDC and OSHA guidelines by adhering to strict procedures for handling and washing soiled linens. Always use proper personal protective equipment (PPE), such as gloves and gowns, to reduce the risk of exposure to harmful pathogens. Avoid shaking or agitating linens, as this can release infectious particles into the air.
When it comes to laundering, hot water - set to at least 160°F - combined with an appropriate detergent is essential for sanitizing linens effectively. If hot water isn’t feasible, opt for EPA-approved chemical disinfectants designed for healthcare settings. Make sure linens are dried thoroughly, as damp fabrics can encourage bacterial growth. Once cleaned, store linens in a designated, sanitary space to prevent cross-contamination.
To make infection control even easier, consider disposable solutions like Peelaways bed sheets. These multi-layer sheets let caregivers peel off soiled layers, removing the need for washing while maintaining a clean and hygienic environment.
How can care facilities safely separate and transport clean and soiled linens to avoid cross-contamination?
To minimize the risk of cross-contamination in care facilities, it's crucial to handle clean and soiled linens separately. Always use designated bins or bags for soiled items, making sure they’re clearly labeled to prevent mix-ups. Don’t overfill containers - this helps reduce the chances of spills or accidental exposure.
For a more hygienic and hassle-free option, products like Peelaways disposable sheets can be a game-changer. These multi-layer sheets eliminate the need for washing, simplify linen handling, and significantly lower the risk of cross-contamination.
Related Blog Posts
- 5 Steps for Handling Contaminated Linens Safely
- How Disposable Sheets Reduce Cross-Contamination
- How to Prevent Cross-Contamination in Bedding
- Checklist for Reducing Laundry in Hospitals
Comments
0

SAVE MONEY & WATER
Professionals & Institutions save a fortune on labor/laundry.

SUPERIOR COMFORT
The first thing our customers notice is how soft our sheets are.
100% WATERPROOF
Each layer is 100% Waterproof, perfect for spills and accidents

SAVE TIME
Change the sheet in under 1 minute without stripping the bed.




Leave a comment