How Incontinence Disrupts Sleep Patterns

Living with incontinence can severely disrupt your sleep, impacting your physical and emotional well-being. Here's how it affects your nights and what you can do about it:
- Frequent wake-ups: Getting up multiple times to use the bathroom interrupts deep sleep stages, leaving you groggy and tired.
- Discomfort from leaks: Wet bedding causes skin irritation and prolonged cleanup, keeping you awake longer.
- Stress and anxiety: Worrying about accidents can delay sleep and lead to fragmented rest.
Solutions include managing fluid intake, creating a safe bedroom setup, and using tools like PeelAways disposable sheets to reduce cleanup time. If symptoms persist, consult a healthcare provider to explore treatment options and improve your quality of life.
Sleep Interrupted: How Nighttime Urination Impacts Your Rest and What You Can Do About It
How Incontinence Disrupts Sleep Patterns
Incontinence can wreak havoc on sleep through three main challenges: waking up repeatedly, dealing with the discomfort of wet bedding and skin irritation, and managing the mental strain of constant worry. Combined, these factors make it difficult to achieve a restful night's sleep.
Frequent Awakenings and Sleep Fragmentation
Each time you wake up to use the bathroom or handle a leak, your sleep cycle is interrupted. This can prevent you from reaching the deeper stages of sleep, like REM and deep sleep, which are essential for feeling refreshed. Losing out on these stages leaves you groggy and less rested the next day [2][6][7].
The frequency of these interruptions also matters. While waking up once during the night might not seem like a big deal, waking up two or more times is linked to worse sleep quality and increased daytime fatigue [3][6]. A Stanford study on women with urgency urinary incontinence found that 57% experienced poor sleep quality, with participants averaging 1–2 nightly trips to the bathroom before seeking treatment. Their average Pittsburgh Sleep Quality Index score was 6.4, indicating significant sleep disruption [3].
Each interruption can last several minutes, reducing your overall sleep time. Instead of the recommended 7–9 hours of consistent rest, you might only get 4–5 hours of broken, light sleep [9][5][6]. Research has shown that individuals with overactive bladder and urinary incontinence report higher levels of sleep disturbances and fatigue compared to those without these conditions [2][7]. The severity of symptoms often directly correlates with the extent of sleep disruption. Studies of older adults and nursing home residents have confirmed that nighttime incontinence episodes are among the strongest predictors of sleep problems, including difficulty staying asleep and waking too early [5][10].
Beyond these interruptions, the physical discomfort caused by incontinence further compounds the problem.
Discomfort from Leaks and Wet Bedding
Physical discomfort is another major factor disrupting sleep. The sensation of wetness from leaks can wake even the heaviest sleepers. When urine soaks through clothing or bedding, it creates a cold, clammy feeling that jolts you awake and makes falling back asleep much harder [9][5].
Prolonged exposure to moisture can also irritate the skin. Urine breaks down the skin's protective barrier, leading to itching, burning, and conditions like incontinence-associated dermatitis. These skin issues can be painful enough to disrupt your sleep, even on nights without visible leaks [4][5].
One user shared their relief after finding a better way to manage leaks:
"After clean up and I geared away the top layer, nothing. I mean nothing soaked, seeped through, not even smell." - Stephanie Jackson [1]
This highlights a common struggle: leaks not only disrupt sleep but also create a cascade of tasks - changing pajamas, stripping the bed, and cleaning up - which can take 15 minutes or more, leaving you fully awake.
For older adults or those with limited mobility, these challenges are even greater. They may have difficulty quickly addressing accidents, leading to prolonged skin exposure to moisture. This increases the risk of painful skin breakdown, which can further interfere with sleep quality [5][10]. Caregivers, too, face disrupted sleep due to frequent nighttime linen changes and skin care routines.
"These have saved my sanity! With 2 incontinent special needs teenagers... these have relieved a lot of stress. They hold a LOT of liquid and are easy to use and tear away. No more 15 loads of laundry and wet mattresses!" - Jalene Stanger [1]
Stress and Anxiety About Bedwetting
The fear of leaks can be just as disruptive as the leaks themselves. Many people with incontinence experience anticipatory anxiety - lying awake, monitoring their bladder, and worrying about potential accidents, odors, or stains. This is especially stressful when sharing a bed or bedroom [9][5].
This constant worry leads to behaviors like excessive fluid restriction and frequent, unnecessary bathroom trips.
"I was going away to visit family and was so worried about my bladder leakage at night. I didn't want to ruin their bed..." - Diana L. Magda [1]
Such anxiety takes a toll over time. Studies have found strong links between sleep disturbances and higher levels of depression, anxiety, and stress in people with overactive bladder [2]. Poor sleep and chronic fatigue can worsen stress, which in turn exacerbates bladder symptoms and perceived urgency [2][4]. Stress hormones and heightened nervous system activity can make the bladder more reactive, while mood changes like depression can reduce motivation to stick to treatment plans or helpful lifestyle strategies [2][4].
The emotional effects often extend beyond the bedroom. Both children and adults can feel embarrassed about nighttime accidents, adding another layer of psychological distress to an already challenging situation.
"When he has an accident he now can take care of it himself and put a new top sheet on his bed. No more scrubbing, no more smell, and no more embarrassment." - Ronda [1]
This creates a vicious cycle: incontinence disrupts sleep, poor sleep worsens symptoms and mental health, and increased stress further damages sleep. Breaking this cycle requires addressing both the physical symptoms and the emotional challenges at the same time [2][6][7]. Together, these disruptions highlight the need for a comprehensive approach to help restore uninterrupted sleep.
Common Sleep Problems Linked to Incontinence
Incontinence can wreak havoc on sleep patterns, ultimately affecting overall health. These disruptions often appear as insomnia and poor sleep efficiency, creating a cascade of challenges.
Insomnia and Poor Sleep Efficiency
Living with incontinence can make falling and staying asleep a challenge. The constant worry about potential leaks can keep you on edge at bedtime, making it hard to relax [5]. During REM sleep, when pelvic muscles are naturally more relaxed, bladder control decreases, increasing the risk of leakage and sleep interruptions [11][4].
Nocturia - waking up multiple times during the night to urinate - is another major disruptor. According to the International Consultation on Incontinence Research Society, waking two or more times per night is considered clinically significant. This not only interrupts sleep but also reduces its efficiency and leaves you feeling groggy during the day [3][6]. Studies have consistently linked frequent nighttime urination to dissatisfaction with sleep quality, highlighting nocturia's impact [2].
The aftermath of nighttime accidents, like cleaning up or changing bedding, can further delay your return to sleep, robbing you of those crucial restorative hours.
Daytime Fatigue and Reduced Quality of Life
Broken sleep often leads to daytime fatigue, which affects productivity, focus, and emotional well-being. Research shows that many people with overactive bladder experience persistent exhaustion, even beyond what nocturia alone might explain [2]. This suggests that the fatigue stems from a combination of factors tied to disrupted sleep.
The link between incontinence and fatigue is a two-way street. Poor sleep caused by frequent awakenings can lead to daytime drowsiness, trouble concentrating, and mood swings [2]. Over time, chronic fatigue may even weaken pelvic floor muscles, worsening bladder control and increasing the risk of leakage [11][8]. For those with overactive bladder, there’s a clear connection between poor sleep and the severity of urinary symptoms, which can further diminish overall quality of life [2]. As incontinence worsens, sleep quality declines, creating a cycle that amplifies daytime struggles.
This fatigue doesn’t just stop at tiredness - it can also compound existing health problems.
Connection with Other Health Conditions
Incontinence often overlaps with other health issues like sleep apnea, depression, and chronic pain, creating a vicious cycle of worsening symptoms and poor sleep.
Sleep apnea is particularly tied to incontinence. About half of those with sleep apnea also experience some form of urinary incontinence, often manifesting as nocturia [8]. The relationship is reciprocal: sleep apnea can lead to increased nighttime urine production and heightened bladder sensitivity, further disrupting sleep. Addressing sleep apnea may help reduce nighttime urination and improve both sleep quality and incontinence symptoms [8].
Mental health also plays a role. Depression and anxiety are closely linked to disrupted sleep patterns. Studies show that people with overactive bladder often experience higher levels of depression, anxiety, and stress, which are compounded by frequent nighttime awakenings [2]. The stress of managing incontinence can take a toll on emotional well-being, creating a feedback loop where poor sleep worsens mood disorders, and these disorders, in turn, exacerbate incontinence episodes [5].
Chronic pain and metabolic issues further complicate the picture. Stress and anxiety from sleep loss can worsen these conditions, leading to a broader decline in health. For older adults, frequent awakenings increase the risk of falls, which can result in injuries and other complications [4]. Additionally, urinary tract infections - both a cause and consequence of incontinence - can further disrupt sleep [4].
A study conducted in Australia on older adults living in the community found that urinary incontinence was a unique predictor of sleep complaints, even when other factors were taken into account [5]. This underscores the importance of addressing incontinence to improve overall sleep quality and health.
Practical Solutions for Better Sleep With Incontinence
Dealing with nighttime incontinence can disrupt your rest, but there are practical steps to address this challenge. By making a few adjustments to your daily habits and creating a more accommodating sleep environment, you can reduce disturbances and enjoy better sleep.
Daily Habits to Support Sleep
Start by managing your fluid intake. Drinking plenty of water during the day is important, but try to limit fluids 2–3 hours before bedtime. This helps reduce nighttime trips to the bathroom without compromising hydration during the day.
Avoid caffeine and alcohol in the evening. Both act as diuretics, increasing urine production, which can lead to more frequent wake-ups. It’s a good idea to stop consuming caffeinated drinks by mid-afternoon. Instead, opt for water or herbal tea later in the day.
Another key habit is sticking to a consistent sleep schedule. Going to bed and waking up at the same time every day - even on weekends - helps regulate your body’s internal clock and supports bladder control. Make it part of your routine to empty your bladder completely before bed to minimize early-night urges.
Studies suggest that waking up once during the night to use the bathroom is manageable for most people. However, getting up two or more times can significantly affect sleep quality, leaving you feeling groggy and tired during the day.
Once your daily habits are in check, focus on creating a bedroom setup that minimizes disruptions.
Creating a Comfortable and Safe Sleep Environment
Your sleep environment plays a huge role in managing interruptions caused by incontinence. Start by ensuring your bedroom is safe and easy to navigate at night. Install nightlights or motion-activated lights to illuminate your path to the bathroom without fumbling for a switch in the dark. This is especially important for older adults to prevent falls.
Remove potential tripping hazards like loose rugs, cords, or clutter. For those with mobility issues, consider placing a bedside commode nearby to reduce the distance needed to reach a bathroom.
Keep your bedroom cool - ideally between 60–67°F - for better sleep. Protect your mattress with waterproof or absorbent sheets to avoid the discomfort of dealing with soaked bedding. This small step can make a big difference in maintaining a restful night.
PeelAways: A Simple Solution for Bed Protection
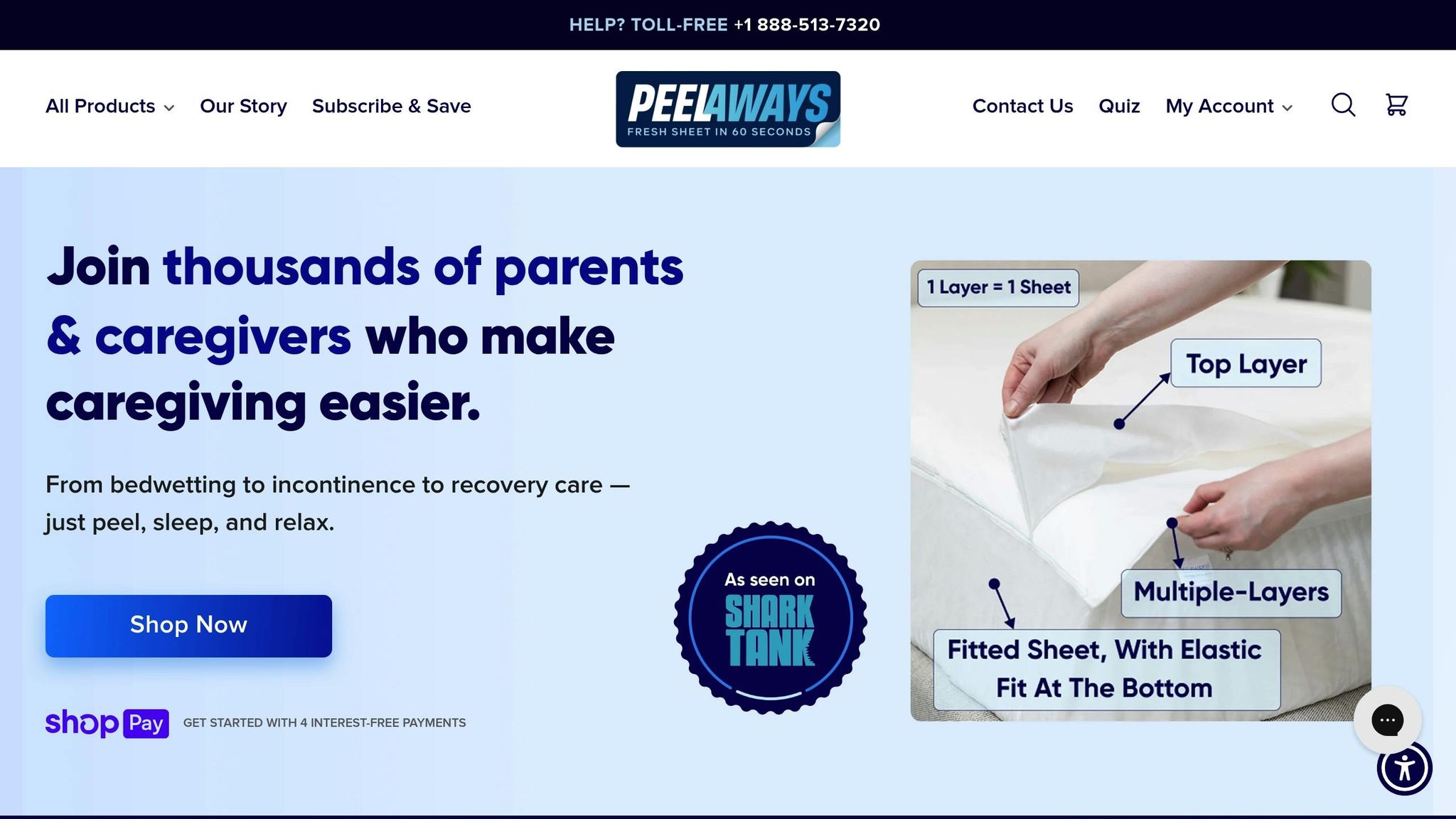
One product worth considering for managing incontinence is PeelAways. Traditional waterproof mattress pads often require frequent washing, which can add stress and time to your routine. PeelAways offers an alternative with its innovative multi-layer, disposable waterproof fitted sheets.
Each PeelAways sheet contains 5 to 7 absorbent layers, depending on the size. For example, Cot and Twin XL sizes include 7 layers, while other sizes come with 5. When an accident happens, simply peel off the soiled top layer to reveal a clean one underneath. This process takes less than a minute and eliminates the need to lift the mattress or strip the bed entirely.
The sheets are made with soft, breathable fibers and feature an advanced membrane base that blocks liquids while allowing airflow. This keeps your bed cool and dry. Plus, each layer is completely waterproof, preventing leaks from reaching the mattress.
"I couldn't believe these would be waterproof from accidents because the linings were so thin, but was I wrong. They do not seep through to the next liner and are so much easier to use than changing sheets every day for the elderly." – Linda
For caregivers, PeelAways can be a game-changer. Instead of handling heavy, wet bedding multiple times a week, caregivers can simply peel off a layer and dispose of it. This reduces physical strain and lowers the risk of cross-contamination.
PeelAways can be used discreetly under regular bedding or on their own. They are free from Vinyl, PVC, Phthalates, and fire retardants, making them odorless and gentle on sensitive skin. Available in various sizes - including Crib-A-Peel for toddlers ($30.99), Cot ($34.99), Twin ($34.99), Twin XL with 7 layers ($41.99), Full ($43.99), Queen ($47.99), and King ($53.99) - they cater to a range of needs, from potty training to elder care.
For children or teenagers, PeelAways can also provide a sense of independence. They allow kids to handle accidents on their own without needing to wake a caregiver, which can reduce embarrassment and build confidence.
"My 12-year-old son doesn't wake up sometimes and has accidents. These sheets are the perfect solution. They protect his mattress and are discreet under his regular bed sheets. It has helped so much. When he has an accident, he can now take care of it himself and put a new top sheet on his bed. No more scrubbing, no more smell, and no more embarrassment." – Ronda
sbb-itb-45288fe
When to Consult a Healthcare Professional
While lifestyle changes can help manage incontinence and sleep issues, there are times when medical advice becomes essential. Persistent symptoms or certain warning signs should prompt you to seek professional care.
If you’re waking up two or more times each night, it’s a sign that your sleep quality might be suffering. This level of disruption can leave you feeling drained during the day and interfere with daily activities. It’s a good idea to reach out to your healthcare provider if this is happening to you [6].
Other symptoms that warrant immediate attention include sudden onset of incontinence, pain or burning during urination, blood in your urine, unusual odors, unexplained weight loss, fever, severe pelvic or abdominal pain, sudden inability to urinate, or signs of dehydration. Additionally, new numbness, leg weakness, bowel changes, or back pain should not be ignored.
For those with sleep apnea, it’s worth noting that about half of sufferers also deal with urinary incontinence. Addressing sleep apnea - especially if you’re experiencing symptoms like loud snoring, gasping for air during sleep, or feeling excessively sleepy during the day - can improve incontinence as well [8]. Be sure to discuss these concerns with your doctor.
Medications can also play a role in nighttime incontinence. Drugs like diuretics, sedatives, antidepressants, and blood pressure medications might contribute to the issue. A review of your prescriptions with your doctor can help pinpoint any potential culprits. For example, taking diuretics earlier in the day rather than in the evening may help reduce disruptions at night.
Incontinence can also take an emotional toll, leading to stress, anxiety, or even depression. If you’re feeling overwhelmed, consider seeking professional help for therapy that focuses on managing both sleep and emotional well-being.
To prepare for your appointment, keep a bladder diary for 2–3 days. Note the times you urinate, the approximate volume, any incontinence episodes, the types and amounts of fluids you consume, your sleep schedule, and any medications you’re taking. This record can provide valuable insights for your healthcare provider and help them develop an effective treatment plan.
Given the impact of incontinence on sleep, your first step should be consulting your primary care provider. They may refer you to specialists like a urologist, urogynecologist, geriatrician, or sleep specialist. During your evaluation, expect a thorough review of your medical history, a physical exam, and possibly tests such as a urinalysis, urine culture, or blood work.
For caregivers, it’s important to seek medical advice if a loved one is waking frequently at night, appears overly tired or confused, shows signs of skin irritation or infections, or is at risk of falling while trying to reach the bathroom. These signs indicate the need for professional guidance.
Conclusion
Living with incontinence doesn't mean you have to settle for restless nights and poor sleep. Research clearly shows that effectively managing incontinence can significantly improve sleep quality, reduce daytime fatigue, and boost overall well-being. Studies highlight that proper interventions can minimize sleep disturbances and enhance quality of life [3][5].
The connection between incontinence and sleep is a two-way street. Addressing incontinence not only lessens nighttime accidents but also helps break the cycle of disrupted sleep, stress, and worsening symptoms. For instance, research suggests that appropriate treatments can reduce nighttime bathroom visits from multiple trips to just once - or even eliminate them entirely - leading to better, uninterrupted sleep [3]. This improvement also carries over into the day, easing the depression, anxiety, and stress often linked to sleep issues [2].
Taking action is key. Whether it's consulting with a healthcare provider, adjusting daily routines, or using practical tools to protect your bedding, each step brings you closer to restful nights. Waking up multiple times during the night disrupts your sleep cycles and affects your overall quality of life, so it’s important to seek professional advice when needed [3].
For many, practical solutions like protective bedding can make an immediate difference. Accidents can lead to soaked clothes, wet mattresses, and lingering odors, which not only disturb sleep but also create anxiety about future incidents [5]. Products like PeelAways provide a simple and effective solution. Their multi-layer bedding design allows you to quickly remove soiled layers without the hassle of remaking the bed, offering relief and convenience.
With over 12,000 satisfied customers and an impressive 4.8 average rating, PeelAways has become a trusted choice for caregivers and individuals seeking to reduce the stress and time involved in managing nighttime incontinence.
Improved sleep starts with recognizing that you have options. You don’t have to accept disrupted nights as your reality. By combining medical advice, lifestyle changes, and practical solutions like protective bedding, you can tackle the physical challenges, discomfort, and emotional strain caused by incontinence. Regaining control over your nights means reclaiming your energy and improving your quality of life.
Related Articles
Check out these helpful resources for practical ways to manage nighttime incontinence and improve sleep quality. Each one focuses on a specific aspect of handling incontinence during the night.
How to Choose the Best Waterproof Bedding for Nighttime Accidents
The right waterproof bedding can make a world of difference in your sleep and peace of mind. This guide breaks down what to look for - like 100% waterproof protection, breathability, comfort, and ease of use. It also explains how multi-layer disposable options can save you time, reduce laundry, and support overall health. With insights from over 8,000 satisfied users who’ve said goodbye to wet mattresses and endless sheet changes, this article offers clear, practical advice to help you pick the best option for your needs.
Read more: How to Choose the Best Waterproof Bedding for Nighttime Accidents
Top Tips for Caregivers Managing Incontinence at Night
Caring for someone with nighttime incontinence can be tough, especially when it disrupts sleep for both the caregiver and the person they’re helping. This article shares practical tips to make nighttime management easier, like layering protective bedding, keeping supplies within arm’s reach, and reducing fall risks during late-night bathroom visits. It also highlights ways to cut cleanup time and protect your own rest. Since studies link sleep disruptions and caregiver fatigue to worse incontinence symptoms and lower quality of life, these strategies aim to ease stress and improve sleep for everyone involved.
Read more: Top Tips for Caregivers Managing Incontinence at Night
The Psychological Impact of Incontinence and How to Cope
Nighttime incontinence doesn’t just affect sleep - it can take a toll on mental health, too. Research shows that the fatigue and sleep disturbances caused by incontinence are often tied to higher levels of depression, anxiety, and stress. This article dives into the emotional challenges of living with incontinence, like embarrassment, fear of accidents, and the anxiety that can make falling asleep harder. It also offers practical and emotional coping strategies to help you rebuild confidence and reduce the mental strain that can worsen sleep problems.
Read more: The Psychological Impact of Incontinence and How to Cope
FAQs
What are some practical ways to reduce sleep disruptions caused by incontinence?
Managing sleep disruptions caused by incontinence can be made easier by creating a more comfortable and low-stress environment. A smart option to consider is Peelaways disposable, waterproof bed sheets, which feature a multi-layer peel-away design. If one layer gets soiled, you can simply peel it off to reveal a fresh, clean sheet - no need for washing or struggling with the mattress.
These sheets are a practical way to reduce nighttime stress and discomfort, helping to maintain a clean and restful sleep space. They’re particularly helpful for caregivers and families dealing with elder care, medical recovery, or potty training.
What can caregivers do to minimize sleep disruptions caused by incontinence for themselves and those they care for?
Caregivers looking to minimize nighttime interruptions caused by incontinence can benefit from practical tools like Peelaways disposable bed sheets. These sheets feature multiple layers that are waterproof, soft, and breathable, making them both comfortable and convenient. When the top layer becomes soiled, simply peel it away to expose a fresh, clean layer beneath - no need for lifting mattresses or dealing with late-night laundry.
This thoughtful design not only cuts down on time and effort but also ensures a cleaner and less stressful sleeping environment for both caregivers and those they care for.
How can Peelaways sheets help improve sleep for people with incontinence?
Peelaways sheets are a game-changer for anyone dealing with incontinence, providing a soft, waterproof, multi-layer design that makes nighttime cleanups incredibly simple. Instead of wrestling with traditional sheets, you just peel off the top layer to reveal a fresh, clean surface underneath - no heavy lifting, no laundry, and no extra effort.
This straightforward solution not only keeps nighttime disruptions to a minimum but also eases stress, enhances comfort, and protects your mattress. The result? A cleaner, more comfortable sleep environment that helps you rest easier.
Related Blog Posts
Comments
0

SAVE MONEY & WATER
Professionals & Institutions save a fortune on labor/laundry.

SUPERIOR COMFORT
The first thing our customers notice is how soft our sheets are.
100% WATERPROOF
Each layer is 100% Waterproof, perfect for spills and accidents

SAVE TIME
Change the sheet in under 1 minute without stripping the bed.




Leave a comment