Best Practices for Bedding Hygiene in Group Homes

Maintaining clean bedding in group homes is critical for preventing infections and ensuring resident comfort. Bedding can harbor bacteria, fungi, and viruses from bodily fluids, making proper handling, washing, and storage essential. Here's what you need to know:
- Avoid shaking soiled linens to prevent spreading bacteria into the air. Roll them inward and place directly into leak-proof bags.
- Separate clean and dirty linens at all times. Use distinct zones for handling soiled and fresh laundry.
- Wash at high temperatures (160°F or higher) to kill pathogens.
- Use waterproof mattress covers and inspect them regularly for damage.
- Consider disposable bedding like PeelAways for quick changes and reduced contamination risks.
Caregiver training, proper use of gloves and aprons, and clear protocols are key to maintaining hygiene. These steps protect residents' health, reduce caregiver strain, and improve overall cleanliness.
Infection Control Basics for Healthcare Laundry Services: Part 1
Preventing Cross-Contamination: Core Practices
Addressing the challenges of cross-contamination in group homes requires careful attention to these essential practices.
How to Handle Linens Safely
The way caregivers manage soiled linens plays a big role in infection control. Never shake soiled bedding - this can release harmful microorganisms and lint particles into the air, spreading bacteria like Salmonella and Staphylococcus aureus [1][3]. Instead, roll up soiled linens carefully with the dirty side tucked inward to contain contaminants before placing them in a bag [3].
"Handling contaminated laundry with a minimum of agitation can help prevent the generation of potentially contaminated lint aerosols in patient-care areas." – CDC [1]
When dealing with heavily soiled linens, always wear gloves and aprons for protection [1][2][3]. Avoid carrying soiled linens against your body; instead, place them directly into clearly labeled, leak-proof bags or containers at the point of soiling [1][3]. For linens contaminated with feces or vomit, scrape bulk solids into a toilet using a flat-edged tool before bagging them [3]. After removing personal protective equipment (PPE), practice proper hand hygiene [3][7].
Setting Up Linen Change Schedules
The frequency of linen changes should align with each resident's needs and the level of soiling. To limit bacterial growth, avoid storing used linens for extended periods before washing [2]. Sort linens into three categories: Clean (ready for use), Used (not exposed to body fluids), and Infectious (contaminated with blood, feces, or known infections) [8]. Infectious linens should be bagged immediately at the point of use [8].
For thermal disinfection, wash linens at a minimum temperature of 160°F (71°C) for at least 25 minutes [1]. Alternatively, follow global healthcare guidelines recommending temperatures between 158–176°F (70–80°C) for at least 10 minutes [3]. Wash each resident's personal items separately to avoid cross-contamination [8].
A well-organized schedule, supported by a physical system, can help maintain these practices consistently.
Keeping Clean and Dirty Linens Separate
Strictly separating clean and dirty linens is critical to preventing contamination. Laundry facilities should have two distinct zones: a "dirty" area for receiving and handling soiled items and a "clean" area for processing and folding washed items [1][3].
"Always keep clean and used linen separate... store clean linen above floor level, in a clean, cool, dry place." – UK Health Security Agency [2]
Use dedicated trolleys for clean, used, and soiled laundry to prevent cross-contact [2]. Store clean linens in a cool, dry place above floor level to protect them from dust, debris, or moisture [2]. Implement a "first-in, first-out" system to ensure older linens are used first [2]. Additionally, transport carts should be cleaned and disinfected daily using a neutral detergent and warm water solution [3].
Bedding Solutions for Group Homes
Maintaining hygiene in group homes is critical, especially when caring for vulnerable residents. The following bedding options build on existing cross-contamination controls to ensure safety and comfort.
Waterproof Mattress Covers and Encasings
Waterproof mattress covers are essential for protecting both residents and mattresses from fluids and pathogens. As the CDC defines it, a mattress cover is a fitted, protective layer designed to prevent contamination from body fluids. A standard linen sheet, on the other hand, doesn’t qualify as a protective cover [1].
When choosing a mattress cover, opt for one with a breathable membrane. These covers block liquids while allowing air to circulate, reducing the heat buildup often associated with traditional plastic covers. Regular inspections are crucial - check both sides for signs of moisture, stains, or damage. If any imperfections are found, replace the cover immediately. The FDA highlights the risks of worn or damaged covers, stating that they can allow fluids to seep into the mattress, potentially exposing residents to infections from contaminated materials [9][10].
Disposable Multi-Layer Bedding
Disposable multi-layer bedding is revolutionizing how caregivers manage bed changes in group homes. Products like PeelAways offer 5–7 waterproof layers that simplify the process. Caregivers can peel away the soiled top layer in under a minute, revealing a fresh, clean sheet. This eliminates the need to lift mattresses, strip beds, or handle contaminated linens, significantly reducing the chances of cross-contamination.
Lou Leibhaber, Former Chief Operating Officer at Lehigh Valley Hospital and Health Network, highlights the efficiency of this approach:
"The reduced time in changing these sheets can significantly increase the time hospital staff provides care to its patients. On average, it can take two nurses up to 15 minutes to change a sheet while the patient is in the bed. With PeelAways, it can take one nurse less than a minute" [11].
Each layer is made from bamboo, rayon, and polyester, offering a soft texture - 32% softer than standard sheets. These sheets are free from vinyl, PVC, phthalates, and fire retardants, making them safe for residents with sensitive skin [4][11]. Starting at $34.99 for twin sizes, they provide weeks of clean bedding directly on the bed, minimizing the need to retrieve linens during nighttime accidents [4][5]. This streamlined system not only reduces the time spent changing sheets but also improves overall incontinence care.
Managing Incontinence
Effective incontinence management goes hand-in-hand with maintaining hygiene. For residents who experience frequent accidents, bedding with absorbent, waterproof layers is a must. Multi-layer bedding allows caregivers to respond quickly without disturbing the resident’s rest or exerting unnecessary physical effort.
Each layer features a waterproof membrane that contains fluids, while the absorbent top surface wicks moisture away from the skin [4][5]. When an accident occurs, caregivers can simply peel away the soiled layer, containing the mess without disrupting the resident. This design also reduces caregiver strain and upholds the resident’s dignity [4][6]. Given that contaminated textiles can harbor bacterial loads ranging from 1,000,000 to 100,000,000 CFU per 100 cm², swift containment is critical [1][3].
Training and Compliance for Caregivers
Caregivers play a critical role in preventing cross-contamination, and proper training is essential. Contaminated textiles can carry bacterial loads as high as 100,000,000 CFU per 100 cm² of fabric [1], making consistent education and strict adherence to protocols a top priority.
What Caregivers Need to Learn
Caregivers need to develop expertise in three key areas: linen categorization, safe handling techniques, and proper use of PPE (personal protective equipment). They must distinguish between:
- Clean linen: Washed and ready for use.
- Used linen: Not visibly contaminated by body fluids.
- Infectious linen: Contaminated with blood, feces, or other bodily fluids [8].
The UK Health Security Agency emphasizes:
"It is the responsibility of the person handling linen to ensure it is segregated appropriately" [2].
Safe handling practices are equally important. For example, caregivers should avoid shaking or rinsing soiled items. Instead, they should roll contaminated items inward, keeping the soiled side contained, and place them in labeled, leak-proof containers. Proper PPE usage - such as gloves, aprons, and face protection - must be paired with thorough hand hygiene after handling any linen.
Training should also include thermal disinfection guidelines. For infectious materials, water-soluble bags that go straight into the washer reduce the need to re-handle contaminated items, significantly lowering the risk of exposure [8].
Once these core skills are in place, clear and enforceable protocols are necessary to ensure these practices become second nature.
Creating and Enforcing Protocols
To maintain high standards, robust protocols must guide every step of the process. Written standard operating procedures (SOPs), visual aids in laundry areas, and audit checklists can help ensure that contaminated items are kept separate from clean ones. Clean linens should always be stored in dry, enclosed spaces above the floor.
Workflows should clearly separate dirty receiving areas from clean processing zones [2]. Transport systems must also prevent cross-contamination by using separate or partitioned carts for clean and soiled linens. Additionally, soiled items should never come into contact with floors, lockers, or tabletops [8].
Regular audits are crucial. They not only verify compliance but also help identify potential gaps before they pose infection risks.
Educating Residents and Families
Staff training alone isn’t enough - residents and their families also need to understand and support hygiene protocols. For families doing laundry at home, providing clear home-laundry guidelines is essential. These should outline infection risks and stress the importance of high-temperature washing, which is often beyond the capability of typical domestic washing machines [8].
Encouraging residents to report soiled bedding immediately is another key step. Even items that look clean can carry significant bacterial loads [1]. When families understand why certain measures are in place - like why staff wear gloves or why high-temperature washing is necessary - they’re more likely to cooperate with these procedures, even if it means delicate fabrics might not fare well under such conditions.
sbb-itb-45288fe
Expert-Recommended Practices
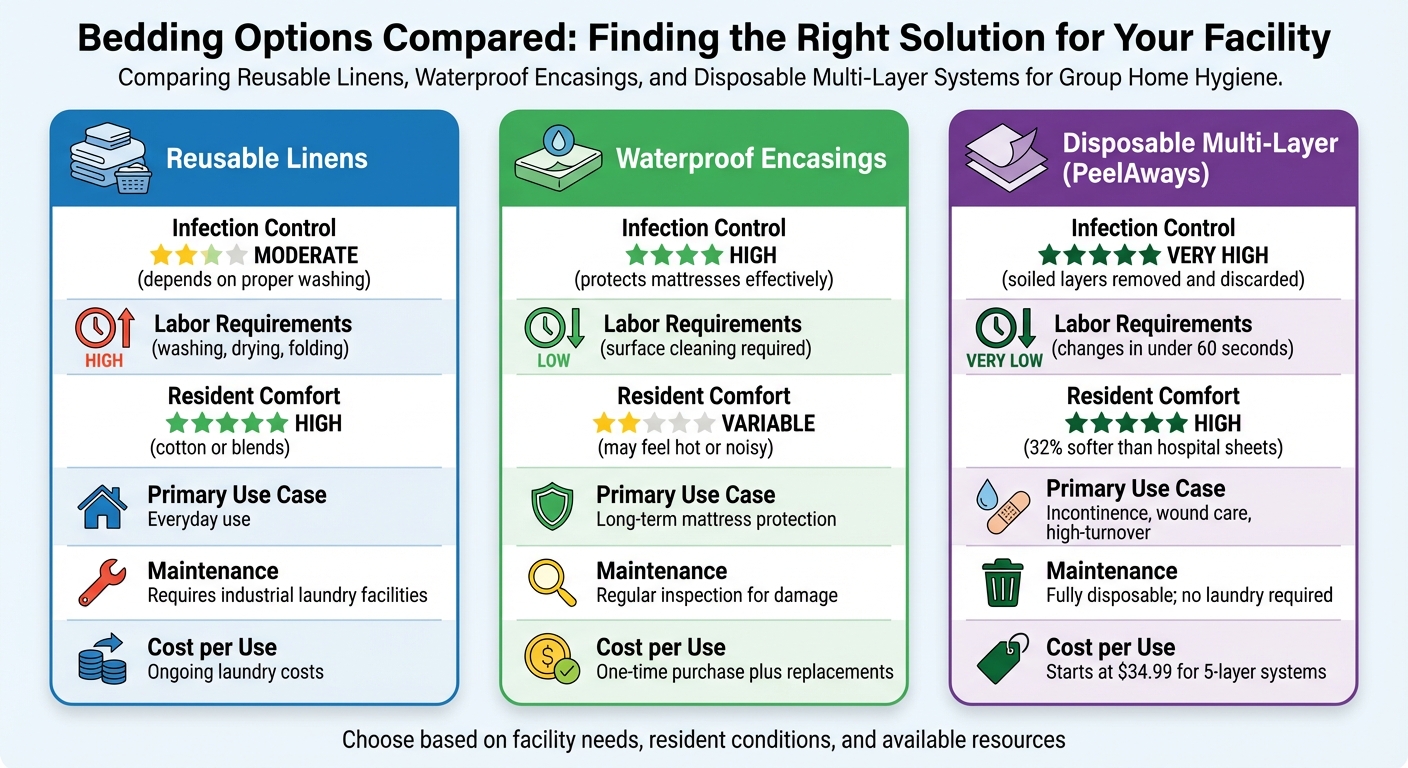
Bedding Options Comparison for Group Homes: Infection Control, Labor and Comfort
10 Best Bedding Hygiene Practices
To maintain top-notch bedding hygiene in group homes, experts recommend a set of practical guidelines. These are backed by the CDC and UK Health Security Agency, emphasizing the importance of proper linen handling to prevent contamination. Studies have shown that textiles can harbor between 1,000,000 to 100,000,000 CFU per 100 cm² of fabric [1].
1. Keep clean and soiled linens separate at all times. Store clean linens in enclosed areas off the floor to prevent contamination [2][8].
2. Avoid shaking soiled bedding. Instead, roll contaminated items inward, ensuring the soiled side is contained [1][3].
3. Wash reusable linens at 160°F (71°C) for at least 25 minutes. For added safety, use chlorine bleach (50–150 ppm) at 135°F–145°F [1].
4. Use waterproof barriers for mattresses. Replace covers immediately if they are torn or cracked, as unprotected mattresses can become breeding grounds for MRSA and other pathogens [1].
5. Consider disposable multi-layer systems to reduce handling and infection risks. Products like PeelAways allow caregivers to quickly remove a soiled layer without lifting the resident, preventing aerosolization. With over 12,000 customer reviews and a 4.61/5 rating, these systems are especially useful for incontinence management [4].
6. Wear proper PPE when handling soiled linens. Use reusable rubber gloves for heavily soiled items to ensure safety [3][2].
7. Use water-soluble bags for infectious linens. Place items contaminated with blood or bodily fluids directly into these dissolvable bags, which can go straight into the washer [8].
8. Remove solid waste at the bedside. Scrape feces or vomit into a toilet before placing the linen in a laundry bag [3].
9. Clean and disinfect laundry equipment daily. Follow manufacturer instructions to prevent microbial buildup in washing machines [1][3].
10. Rotate clean linens using a first-in, first-out system. This ensures older stock is used first, maintaining freshness and efficiency [2].
Bedding Options Compared
The table below breaks down how different bedding options measure up in terms of infection control, labor, and comfort.
| Feature | Reusable Linens | Waterproof Encasings | Disposable Multi-Layer (PeelAways) |
|---|---|---|---|
| Infection Control | Moderate; depends on proper washing | High; protects mattresses effectively | Very High; soiled layers are removed and discarded |
| Labor Requirements | High; involves washing, drying, and folding | Low; surface cleaning required | Very Low; can be changed in under 60 seconds |
| Resident Comfort | High (cotton or blends) | Variable (may feel hot or noisy) | High (soft bamboo/rayon blend, 32% softer than hospital sheets) [6] |
| Primary Use Case | Everyday use | Long-term mattress protection | Ideal for incontinence, wound care, or high-turnover situations |
| Maintenance | Requires industrial laundry facilities | Needs regular inspection for damage | Fully disposable; no laundry required |
| Cost per Use | Ongoing laundry costs | One-time purchase plus replacements | Starts at $34.99 for 5-layer systems; 15% off with subscription [4] |
For residents facing frequent incontinence, disposable multi-layer systems are a game changer. They eliminate late-night laundry runs and provide a clean, waterproof surface in under a minute [4][6]. While reusable linens are still suitable for daily use, they demand strict adherence to thermal disinfection protocols to ensure safety and hygiene.
Conclusion
Maintaining proper bedding hygiene is crucial for protecting residents from infections while upholding their dignity. Every decision about how linens are handled directly influences resident health and well-being.
The essential practices highlighted in this guide - such as separating clean and soiled linens, avoiding the shaking of contaminated bedding, washing at temperatures of 160°F (71°C), and using waterproof barriers - serve as the backbone of effective infection control. Handling linens with care minimizes the risk of pathogen spread and cross-contamination, addressing the high microbial load found in these settings. That said, implementing these protocols requires both comprehensive training and access to the right resources.
Innovative products like PeelAways are changing the game in bedding management. These multi-layer sheets allow caregivers to replace soiled bedding in under 60 seconds without lifting residents or stripping the bed. Their waterproof barrier prevents fluid penetration, reducing bacterial growth and contamination risks. With over 12,000 customer reviews averaging a 4.61/5 rating and being named "Caregiver Product of the Year" [4], these disposable bedding solutions have demonstrated their effectiveness in practical care settings.
By combining these advanced products with strict hygiene protocols, group homes can take a holistic approach to bedding care. Caregivers can spend more time tending to residents’ needs rather than managing laundry, while residents enjoy a cleaner, more comfortable sleeping environment with minimal physical disruption.
Adopting these expert practices not only improves infection control but also lightens the workload for caregivers and enhances resident satisfaction. Investing in better bedding hygiene leads to healthier residents, less caregiver fatigue, and a safer, more efficient care environment overall.
Related Articles
Looking to dive deeper into bedding hygiene and incontinence management? These articles offer practical advice and solutions tailored to group home settings. They complement the strategies discussed earlier, providing a broader perspective on managing these challenges effectively.
- How to Choose the Right Bedding for Incontinence Management – This guide helps you pick bedding that strikes the perfect balance between waterproof protection and comfort for residents. It breaks down the key factors to consider when selecting practical bedding options.
- Simplifying Caregiver Workloads with Multi-Layer Bedding – Discover how multi-layer bedding can make a caregiver's job easier. Learn how it allows bedding changes in under 60 seconds without the hassle of stripping the bed, offering a smarter way to handle daily caregiving tasks.
- Top Benefits of Disposable Bedding in Healthcare Settings – This article highlights how disposable bedding enhances infection control. It explores how reducing laundry handling and transport minimizes cross-contamination risks, while waterproof barriers protect mattresses in healthcare environments.
These resources offer actionable insights to improve both resident care and caregiver efficiency.
FAQs
How often should bedding be changed in group homes to ensure proper hygiene?
In group homes, it's important to change bedding at least once a week to keep things clean and hygienic. If bedding gets soiled - whether from wetness, urine, feces, vomit, or blood - it should be replaced right away. This practice not only helps stop germs from spreading but also creates a more comfortable and sanitary space for residents.
What are the advantages of using PeelAways disposable multi-layer bedding in group homes?
PeelAways disposable multi-layer bedding is a game-changer for group homes, offering convenience and practicality. Each sheet is designed with 5 to 7 absorbent layers that can be peeled away one at a time, revealing a fresh, clean surface. The best part? There's no need to lift heavy mattresses or disturb the resident, making it easier on caregivers and minimizing physical strain. Plus, it eliminates laundry altogether - saving time, water, and detergent expenses.
The built-in waterproof barrier adds an extra layer of protection by safeguarding the mattress and reducing the risk of cross-contamination. This makes it a smart choice for maintaining hygiene and preventing infections. Whether in elder care, special needs facilities, or medical recovery settings, PeelAways provides a straightforward way to keep bedding clean and residents comfortable.
Why is washing bedding at high temperatures important in group homes?
Washing bedding at elevated temperatures is crucial in group home settings to maintain hygiene and ensure effective disinfection. The use of high heat eliminates bacteria, viruses, and other harmful pathogens, significantly reducing the risk of cross-contamination among residents.
This approach is particularly important in shared living spaces, as it helps curb the spread of infections and supports a cleaner, safer environment for all.
Comments
0

SAVE MONEY & WATER
Professionals & Institutions save a fortune on labor/laundry.

SUPERIOR COMFORT
The first thing our customers notice is how soft our sheets are.
100% WATERPROOF
Each layer is 100% Waterproof, perfect for spills and accidents

SAVE TIME
Change the sheet in under 1 minute without stripping the bed.




Leave a comment