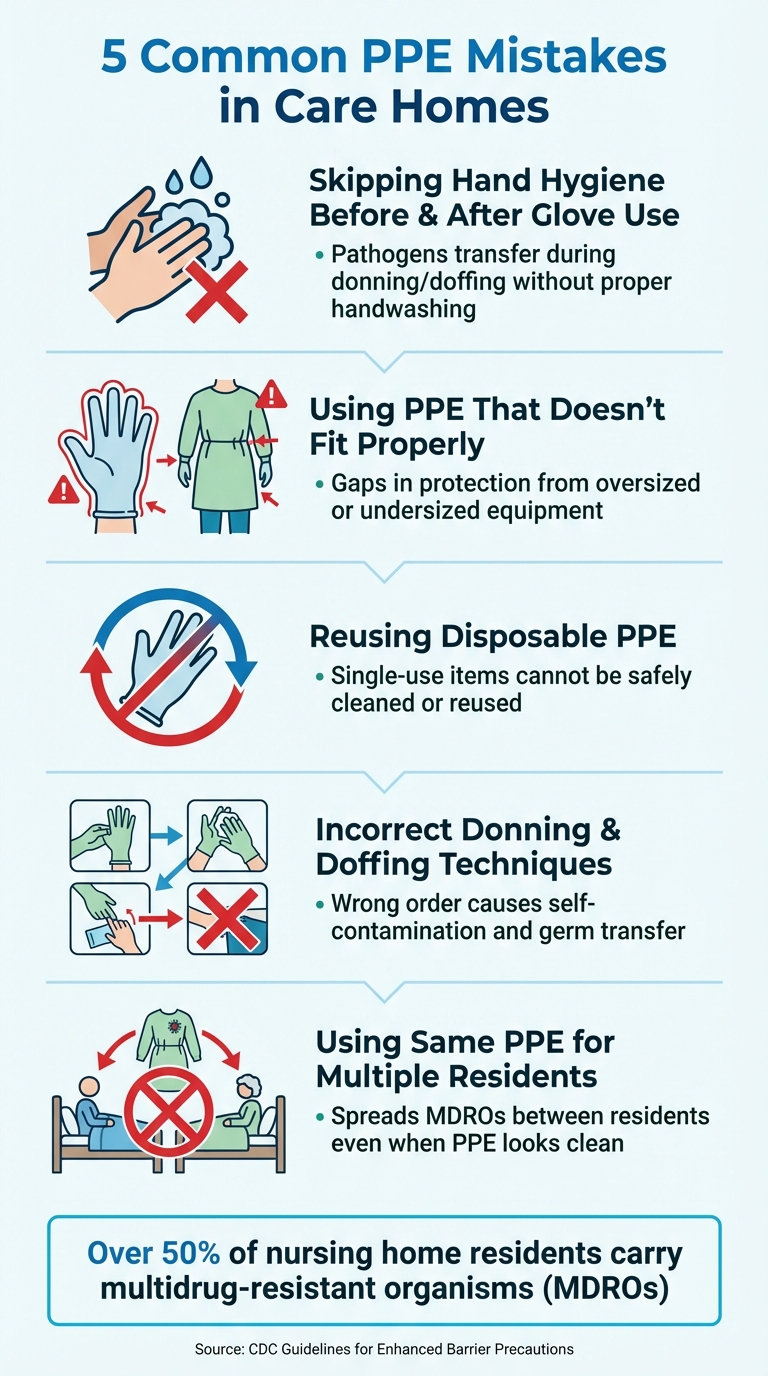
Common PPE Mistakes in Care Homes

Protecting caregivers and residents in care homes starts with proper PPE use. However, common mistakes - like skipping hand hygiene, reusing disposable items, or using incorrect donning techniques - can compromise safety and increase the spread of harmful pathogens, including multidrug-resistant organisms (MDROs). This silent transmission often occurs during routine tasks like dressing or bathing residents.
Here’s what you need to know:
- Hand Hygiene: Always wash hands before and after glove use. Gloves alone aren’t enough to prevent contamination.
- Proper Fit: Ill-fitting gloves or gowns leave gaps, reducing protection.
- Single-Use Only: Reusing disposable PPE spreads pathogens. Discard after each use.
- Correct Removal: Improper doffing can transfer germs to skin or clothing.
- Resident-Specific PPE: Never use the same PPE for multiple residents, even if it appears clean.
To minimize errors, care homes should ensure regular staff training, maintain adequate PPE supplies, and provide practical solutions like disposable hygiene products (e.g., PeelAways sheets) to reduce contamination risks. These steps not only protect caregivers but also improve the overall care environment for residents.
5 Common PPE Mistakes in Care Homes and How to Avoid Them
PPE Done Wrong
Common PPE Mistakes in Care Homes
Even with clear protocols, staff in care homes can sometimes make critical errors when using personal protective equipment (PPE) during resident care [4].
Skipping Hand Hygiene Before and After Glove Use
One of the most frequent mistakes is neglecting hand hygiene. Many caregivers rely solely on gloves, forgetting to wash their hands before putting them on and after taking them off [4]. Without proper handwashing, pathogens can transfer during these steps, turning gloves into a source of contamination rather than protection.
Using PPE That Doesn’t Fit Properly
Wearing PPE that doesn’t fit correctly can reduce its effectiveness. For example, gloves that are too large may slip off, exposing the skin, while gowns that are too small can leave gaps for contaminants [7]. To ensure full protection, staff need access to PPE in various sizes and types that suit different tasks and body shapes.
Reusing Disposable PPE
Disposable PPE is designed for single use only. Reusing items like gloves or gowns, or attempting to clean them, creates unsanitary conditions and increases the risk of spreading pathogens [4][7]. Once PPE is contaminated, it cannot be safely reused and should be discarded immediately.
Incorrect Donning and Doffing Techniques
The order in which PPE is put on and removed is crucial to avoid self-contamination. For instance, taking off gloves before gowns or touching the face with contaminated gloves can transfer harmful germs [4]. Mistakes like these not only reduce the effectiveness of PPE but can also lead to the spread of infections, especially when moving between residents.
Using the Same PPE for Multiple Residents
Each resident requires fresh PPE. One of the most dangerous practices is reusing the same gloves, gowns, or other equipment when caring for multiple individuals. This can lead to the direct spread of multidrug-resistant organisms between residents [4]. Even if PPE looks clean, it may still carry unseen pathogens. Caregivers should always use new PPE for each resident, particularly during high-contact tasks like bathing, dressing, or changing linens [4]. This practice is essential to prevent cross-contamination and protect residents effectively.
Impact of PPE Mistakes on Care Home Safety
The errors in PPE usage outlined earlier have serious consequences for the safety of both residents and staff in care homes. When PPE is used incorrectly, it weakens the protective measures meant to keep everyone safe. One major concern is the high prevalence of multidrug-resistant organisms (MDROs) in these settings. Many residents carry these pathogens without showing symptoms, leading to what the CDC refers to as a "silent spread." This means caregivers can unknowingly transfer harmful bacteria from one resident to another during routine tasks like dressing, bathing, or changing linens [2].
"MDRO transmission is common in skilled nursing facilities, contributing to substantial resident morbidity and mortality and increased healthcare costs." - CDC [2]
Caregivers themselves face significant risks. High-contact activities can transfer MDROs to their hands and clothing, even when contamination isn’t visible [2][3]. A single mistake in PPE use can have lasting effects, as MDRO colonization can persist for months [2]. These risks don't just stop at the caregivers - they ripple out to affect the daily lives of residents.
Improper PPE practices can also harm residents' quality of life. For example, reusing disposable PPE or not donning it correctly doesn’t just increase exposure risks for caregivers; it also limits residents’ ability to engage socially and comfortably. Misapplying strict Contact Precautions instead of Enhanced Barrier Precautions can lead to unnecessary restrictions, such as confining residents to their rooms and reducing opportunities for social interaction and group activities [2]. This is particularly challenging for residents with dementia or hearing impairments, as face masks can hinder communication and increase stress [9].
On a larger scale, mistakes in PPE use disrupt the overall care environment. When PPE isn’t readily available outside resident rooms, staff compliance drops significantly [2][3]. This lack of proper implementation, combined with contaminated clothing or mishandling soiled linens, opens multiple pathways for pathogens to spread. These pathogens can travel through common areas, workstations, and shared equipment, further compromising the safety of everyone in the facility [3].
sbb-itb-45288fe
How to Prevent PPE Mistakes
Avoiding PPE errors in care homes requires a comprehensive strategy that tackles training gaps, supply issues, and heavy workloads. These steps aim to strengthen existing PPE protocols and enhance overall safety.
Training and Regular Refresher Courses
Consistent training is key to ensuring staff understand how to properly use PPE. As guidelines evolve, ongoing education helps caregivers stay updated on best practices. Special emphasis should be placed on high-contact tasks like dressing, bathing, transferring residents, and changing linens - situations where germs can easily spread [2]. It's crucial for staff to use PPE correctly and consistently, even when residents appear to be in good health.
"Effective implementation of EBP requires staff training on the proper use of personal protective equipment (PPE) and the availability of PPE and hand hygiene supplies at the point of care." – CDC [2]
To align with national standards, facilities should encourage staff to complete the CDC's free Nursing Home Infection Preventionist Training. Regular observational audits can pinpoint common errors, such as improper donning or removal of PPE, providing opportunities for immediate corrective training. Annual competency assessments also ensure accountability and keep everyone informed [1].
Providing Adequate Supplies and Monitoring Usage
Even the most well-trained staff can't perform effectively if PPE isn't readily accessible. Supplies should be stored in clean, dry areas at room temperature and placed near caregiving activities [8]. Maintaining sufficient stock levels, checking expiration dates, and rotating inventory are all essential steps [8].
Monitoring how PPE is used can reveal potential issues. For instance, if disposable items are being reused or skipped during routine tasks, it could signal a shortage or accessibility problem rather than intentional non-compliance. Conducting regular audits with standardized observation tools helps facilities identify and resolve these gaps quickly [1].
Using Disposable Hygiene Solutions
Handling traditional linens is labor-intensive and carries a higher risk of contamination. Tasks like transporting soiled laundry and washing items that may not be fully sanitized after one cycle can lead to PPE mistakes, especially when staff are overworked [6]. In addition to ensuring adequate PPE supplies, adopting single-use solutions can significantly reduce these risks.
PeelAways disposable bed sheets are a practical alternative, featuring 5 to 7 waterproof layers. Caregivers can simply peel away the top layer after it becomes soiled, revealing a fresh sheet underneath. This minimizes the need for handling contaminated linens and reduces cross-contamination risks [5][6]. With an average rating of 4.8/5 from over 12,000 customers and being named "Caregiver product of the year", these sheets have proven their effectiveness in real-world settings [5].
"These have saved my sanity! With 2 incontinent special needs teenagers... No more 15 loads of laundry and wet mattresses!" – Jalene Stanger [5]
The sheets also feature a 100% waterproof barrier, preventing fluids from seeping through to the mattress or lower layers, which helps contain pathogens at the source [5][6]. By eliminating the need to transport and launder contaminated linens, facilities can reduce multiple pathways for spreading multidrug-resistant organisms (MDROs). PeelAways are available in various sizes, from Crib ($30.99) to King ($53.99), and offer a 15% subscription discount along with free shipping on orders over $100. Caregivers should still wear gloves and aprons when peeling away used layers and dispose of them following proper protocols [10].
Conclusion
Using proper PPE is critical in preventing the spread of infectious agents and safeguarding both caregivers and residents from multidrug-resistant organisms (MDROs). With over half of nursing home residents potentially carrying these organisms, applying Enhanced Barrier Precautions during high-contact tasks - like dressing, bathing, or changing linens - isn't just advisable; it's absolutely necessary [1][2].
To maintain safety, a well-rounded approach is key. This includes regular staff training with annual updates, ensuring PPE is readily available at the point of care, and following proper procedures for putting on and removing protective equipment. Regular monitoring and audits can catch vulnerabilities early, preventing small issues from escalating into outbreaks. Always remember to change PPE between residents and practice hand hygiene both before and after glove use [2].
Practical solutions can further support infection control while easing caregiver responsibilities. For example, PeelAways disposable bed sheets offer a game-changing way to handle soiled linens. In less than a minute, caregivers can peel away the used layer to reveal a clean, waterproof sheet underneath - reducing contamination risks and saving time. With a 4.7/5 star rating and 95% user recommendation, this product has become a favorite among caregivers. As Sharon A., a verified buyer, shared:
"PeelAway sheets make life so much easier for patient care and caregivers. Absolutely a must-have item" [7].
Related Articles
Discover more strategies to improve infection control and caregiving practices. These resources offer valuable insights into PPE use and infection prevention techniques.
- 5 Ways PeelAways Simplifies Caregiving: Learn how disposable bedding can ease staff workload while maintaining hygiene. This article shares practical tips to save time, allowing caregivers to focus more on residents and less on laundry tasks.
- How to Reduce Cross-Contamination in Elderly Care: Explore effective protocols for minimizing pathogen spread. From surface disinfection to managing high-touch activities, this guide tackles the key steps to reduce the risk of transmitting MDROs.
- Choosing the Right Bedding Solutions for Care Homes: Find expert advice on selecting bedding that provides an ideal mix of comfort, durability, and infection control for care home environments.
FAQs
Why is it important to clean your hands before and after wearing gloves in care homes?
Proper hand hygiene plays a key role in preventing infections in care homes. Washing your hands before putting on gloves is crucial to eliminate any germs that might contaminate the gloves and, in turn, be passed on to residents during care. While gloves provide a protective barrier, they don’t make your hands sterile. Tiny defects in the gloves or the process of removing them can allow microorganisms to spread.
Equally important is cleaning your hands after taking off gloves. The outer surface of the gloves may have been exposed to body fluids or contaminated surfaces, and germs can transfer during removal. To prevent these germs from spreading to other residents, surfaces, or even yourself, always wash your hands or use an alcohol-based hand sanitizer both before and after wearing gloves. This simple practice helps ensure a safer and healthier environment for everyone in the care home.
What are the dangers of reusing disposable PPE in care homes?
Reusing single-use PPE can weaken its protective barrier, reducing its ability to block germs effectively. This creates a higher chance of cross-contamination or even self-infection, particularly if the equipment hasn’t been stored or handled properly.
Disposable PPE is specifically made for one-time use to provide the highest level of protection. Reusing it can spread harmful pathogens to surfaces, clothing, or even directly to individuals. To keep environments safe, always dispose of used PPE right away and replace it with new gear when necessary.
How can care homes make sure PPE fits properly for all staff members?
To make sure personal protective equipment (PPE) fits properly for all staff, start by offering a range of sizes and styles for items like gloves, gowns, masks, and other protective gear. Keep PPE in clean, easy-to-access areas so employees can quickly find the right size when needed. For respirators, conduct fit tests before first use, repeat them annually, and whenever new models are introduced. This ensures a proper seal every time the mask is worn.
Provide training on how to correctly put on PPE, and include a quick check process - like having a colleague confirm the fit of masks, gloves, and gowns. Regular refresher sessions and visible reminders can help reinforce correct usage as requirements change. Encourage staff to report any issues with fit and perform routine compliance checks. Having a dedicated PPE coordinator to manage fit testing, availability, and training can help minimize risks and ensure everyone stays safe.
Comments
0

SAVE MONEY & WATER
Professionals & Institutions save a fortune on labor/laundry.

SUPERIOR COMFORT
The first thing our customers notice is how soft our sheets are.
100% WATERPROOF
Each layer is 100% Waterproof, perfect for spills and accidents

SAVE TIME
Change the sheet in under 1 minute without stripping the bed.



Leave a comment