Solutions for Bedwetting in Kids with Autism

Bedwetting is common among children, but for those with autism, it presents unique challenges due to sensory processing issues, reduced bladder awareness, and sleep disturbances. These factors make nighttime dryness harder to achieve and can impact both the child’s emotional well-being and the family’s daily life.
To address this, practical strategies like consistent bedtime routines, moisture alarms, and sensory-friendly tools can help. Products like PeelAways disposable bed sheets simplify cleanup, reduce stress, and support independence by eliminating the need for frequent laundry.
If accidents persist beyond age 7 or occur alongside other symptoms like pain or snoring, consult a healthcare provider to rule out underlying issues. Combining structured habits with tools like PeelAways can make managing bedwetting easier for families navigating these challenges.
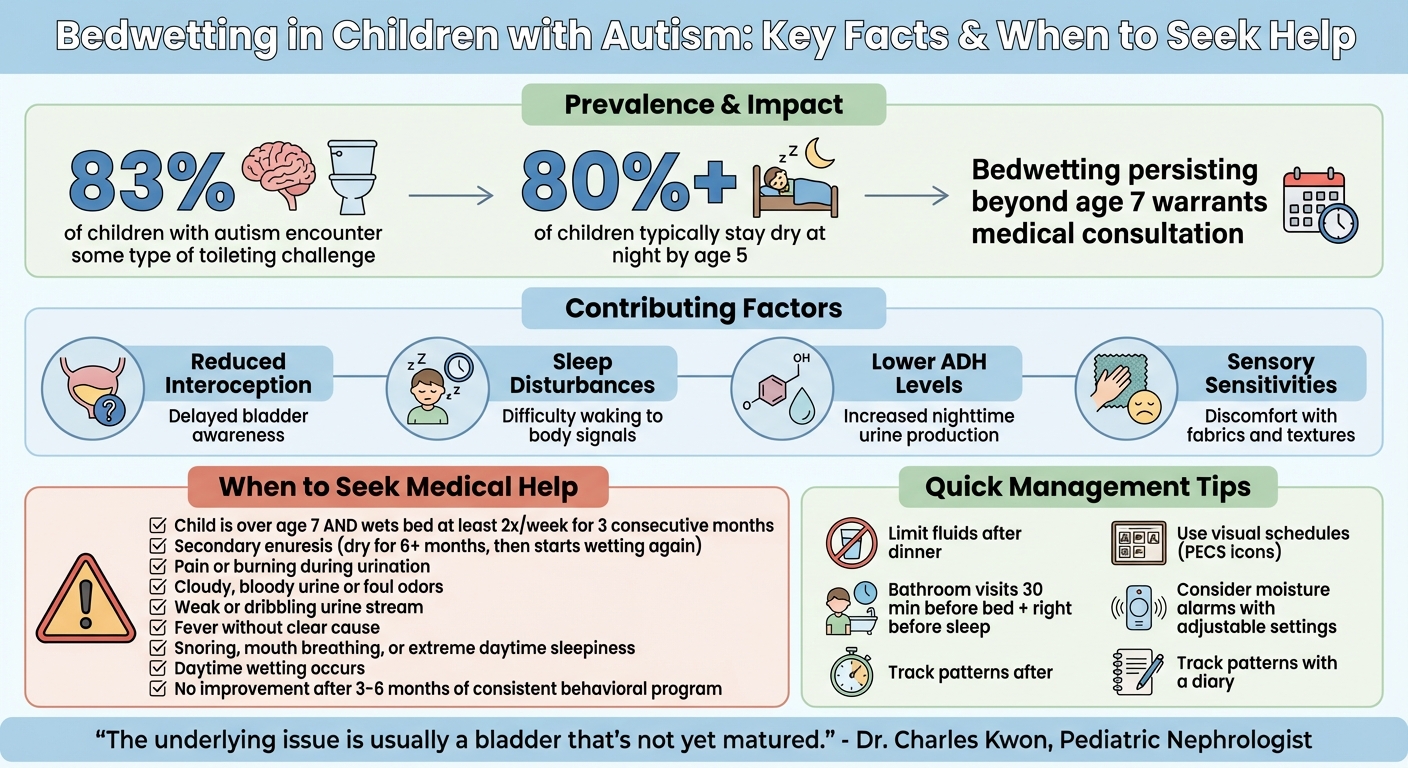
Bedwetting in Children with Autism: Key Statistics and Warning Signs
Why Bedwetting Is More Common in Children with Autism
Sensory Processing and Physical Awareness
For children with autism, reduced interoception - essentially, the ability to sense internal bodily signals - can delay bladder awareness. This means the brain might not recognize the need to urinate in time, making it harder for the child to respond appropriately.
Sleep disturbances add another layer of difficulty. Many children with autism experience disrupted sleep patterns or challenges with self-regulation, which can prevent them from waking up when their body signals the need to use the bathroom. On top of that, some may produce more urine at night due to lower levels of antidiuretic hormone (ADH), further complicating nighttime dryness[1].
Sensory sensitivities also play a role, particularly when it comes to external stimuli. For instance, the feel of certain fabrics, like nighttime underwear or bedding, can be uncomfortable or even distressing. While a neurotypical child might not notice these minor differences, they can create significant discomfort for a child with autism, interfering with both sleep and progress in toilet training[1].
All these sensory challenges not only make nighttime dryness harder to achieve but also contribute to emotional and behavioral struggles for children with autism.
Emotional and Behavioral Effects
Bedwetting doesn’t just pose physical challenges; it can also take an emotional toll, especially for children with autism who may already face difficulties with self-regulation and emotional processing.
Communication barriers often intensify the issue. Around 83% of children with autism encounter some type of toileting challenge[5], and many lack the verbal skills to express their needs or frustrations. This inability to communicate can lead to heightened anxiety, which in turn perpetuates accidents. The stress caused by bedwetting can disrupt carefully established routines - something many children with autism rely on to feel secure and maintain stability.
These combined physical and emotional challenges highlight the complexity of addressing bedwetting in children with autism. It’s not just about managing the physical symptoms but also supporting their emotional and sensory needs.
Practical Strategies to Reduce and Manage Bedwetting
Establishing a Predictable Bedtime Routine
Creating a consistent bedtime routine can play a big role in managing bedwetting. Start by limiting fluids to the morning and early afternoon, and cut back on drinks after dinner to reduce urine production at night. Encourage your child to use the bathroom about 30 minutes before bed and again right before they go to sleep. This helps ensure their bladder is as empty as possible overnight.
Using tools like visual schedules or Picture Exchange Communication System (PECS) icons can make the routine clearer, especially for younger or non-verbal children. These visuals can outline steps like sitting on the toilet, wiping, flushing, and washing hands. For non-verbal kids, you can use a specific sign or a "potty" icon to communicate bathroom needs. If your child struggles with sensory issues, consider accommodations like soft rugs for cold floors or minimizing loud flushing noises. Also, avoid bladder irritants in the evening, such as caffeine, citrus juices, artificial flavorings, and red dyes.
These small but meaningful changes can set the stage for other strategies to support nighttime dryness.
Behavioral Approaches for Nighttime Dryness
When it comes to bedwetting, focus on encouraging your child’s efforts rather than the outcome. For example, praise them for remembering to use the bathroom before bed, as involuntary wetting is often beyond their control. Building on a structured routine, consistent daytime and nighttime habits can help reinforce dry nights. A daytime schedule that includes regular bathroom visits every 2 to 3 hours can develop the skills needed for better nighttime control.
Dr. Laura Kirmayer, a Clinical Psychologist, explains, "The skills training exposure and practice really has to happen in the daytime to see it generalize into the nighttime." [3]
Moisture alarms are another tool to consider. These devices detect the first drops of urine and wake the child, helping them respond to their body's signals. For children with sensory sensitivities, alarms with adjustable volume or vibration features might be more comfortable. However, avoid waking your child randomly during the night, as this can lead to exhaustion without improving bladder control. Keeping a diary of your child’s fluid intake, bathroom visits, and accidents can help you identify patterns or triggers and provide helpful insights if you consult a healthcare provider.
If these strategies don’t show progress, it may be time to consider professional guidance.
When to Seek Medical or Professional Help
If routine and behavioral strategies don’t work, it’s important to seek medical advice. For children over age 7 who wet the bed at least twice a week for three consecutive months, consulting a healthcare professional is recommended [6][7]. By the age of 5, more than 80% of children typically stay dry at night [2], so persistent bedwetting beyond this age may need further evaluation.
Secondary enuresis - when a child who has been dry for at least six months starts wetting again - could point to an underlying issue such as a urinary tract infection, diabetes, or significant emotional stress. Daytime wetting is also unusual and should be assessed by a healthcare provider.
Other warning signs include pain or burning during urination, a weak or dribbling stream, cloudy or bloody urine, foul odors, or fever without a clear cause. If your child develops a fever, seek medical attention within 24 hours to rule out infections. Additionally, bedwetting paired with symptoms like snoring, mouth breathing, or extreme daytime sleepiness might indicate obstructive sleep apnea.
If you’ve tried a structured behavioral program consistently for 3 to 6 months without improvement, it’s time to discuss alternative treatments with a healthcare provider. Be aware that constipation can also contribute to bedwetting in about one-third of children, as it can press against the bladder.
Dr. Charles Kwon, a Pediatric Nephrologist, explains, "The underlying issue is usually a bladder that's not yet matured." [4]
Identifying and addressing any possible medical causes is essential for finding the right solution.
PeelAways Disposable Bed Sheets: A Simple Solution for Bedwetting
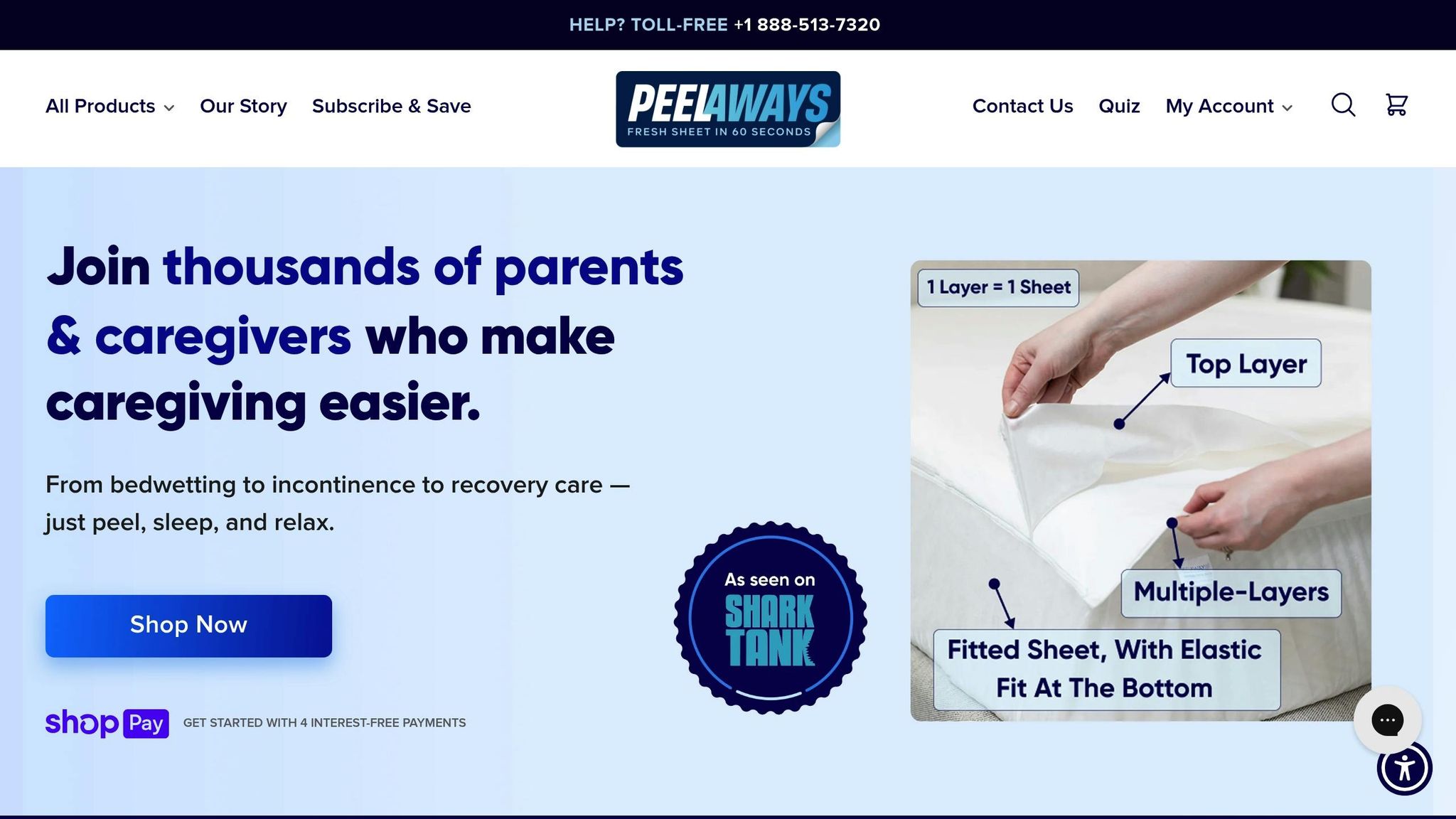
How PeelAways Work
PeelAways provide an easy and efficient way to handle bedwetting, combining practicality with sensory comfort. These sheets feature a patented 5- to 7-layer design that makes cleanup quick and hassle-free [8]. When an accident occurs, you simply peel off the soiled layer, revealing a fresh, clean sheet underneath - all in less than a minute [8]. No more lifting mattresses, wrestling with fitted corners, or late-night bed-stripping marathons.
Each layer is 100% waterproof, ensuring that moisture stays contained and doesn’t seep through to the mattress or other layers below [8]. Made from a soft, breathable blend of bamboo, rayon, and polyester, the sheets feel like traditional fitted sheets - minus the noisy, crinkly texture that can irritate kids with sensory sensitivities [8][10]. Plus, they’re free from harsh chemicals like Vinyl, PVC, Phthalates, and fire retardants [8].
Benefits for Families and Caregivers
For families dealing with bedwetting, especially those with children on the autism spectrum, PeelAways can significantly ease the burden of nighttime accidents. Their peel-away design eliminates the need for frequent laundry, cutting down on up to 15 loads per week. In fact, over 90% of accidents require just a single-layer change [10].
The straightforward design also encourages independence in older children. Many kids can peel away the soiled layer themselves, fostering confidence and reducing embarrassment.
"With 2 incontinent special needs teenagers... these have relieved a lot of stress. They hold a LOT of liquid and are easy to use and tear away. No more 15 loads of laundry and wet mattresses!" - Jalene Stanger [9]
"When he has an accident he now can take care of it himself and put a new top sheet on his bed. No more scrubbing, no more smell, and no more embarrassment." - Ronda [9]
Each layer can last 7–10 days if it remains unsoiled [8]. The breathable fabric also helps avoid the hot, sticky feeling often associated with traditional waterproof mattress protectors.
Available Sizes and Pricing
PeelAways are available in a variety of sizes to fit different beds:
- Crib (52" x 28" x 6") for $30.99 (5 layers)
- Twin (75" x 39" x 6") and Twin XL (80" x 39" x 9") for $34.99, with Twin XL also offered in a 7-layer pack for $41.99 [9][11]
- Full (75" x 54" x 12") for $43.99
- Queen (80" x 60" x 12") starting at $47.99
- King (80" x 78" x 12") for $53.99 [11]
Prices apply to 5-layer packs unless otherwise noted. You can save even more with options like a 15% subscription discount, 5% off 3 packs, or 10% off 6 packs [8]. Plus, orders over $100 qualify for free shipping.
With a 4.61/5 star rating from more than 12,000 customers [8], PeelAways are a practical, sensory-friendly solution that makes bedwetting management easier for families everywhere.
Managing Nocturnal Enuresis
sbb-itb-45288fe
Creating a Comfortable Sleep Environment
Designing a bedroom that feels safe and calming can make a big difference for children with autism who experience bedwetting. A soothing sleep environment can help reduce anxiety and promote better rest. The goal is to create a space that meets their sensory needs and fosters a sense of security. Let’s explore how thoughtful bedding choices and sensory tools can help achieve this.
Selecting Sensory-Friendly Bedding
The right bedding can minimize sensory discomfort and create a secure sleep environment. Look for soft, high-quality fabrics in solid, muted colors like blue, green, or soft brown. Avoid bright patterns or overstimulating designs, as they can overwhelm sensitive children.
"Whether lights are on or off, colors and patterns emit vibrations that affect brain waves in a positive or negative fashion. Because of that, heavy patterns or bright-colored bedding can be overstimulating." – Carolyn Feder, Licensed Interior Designer [12]
Traditional plastic mattress protectors often crinkle and feel uncomfortable, which can be distressing for kids with sensory sensitivities. Instead, choose breathable, fabric-topped waterproof protectors that are quiet and soft to the touch. Products like PeelAways are a great option - they provide multi-layer waterproof protection while feeling like regular fitted sheets, making accident management easier without sacrificing comfort.
Keep the overall bedroom color palette muted and calming. Shades of blue, green, purple, or brown work well, while bright reds, oranges, and stark whites should be avoided as they can be too stimulating. Placing the bed against a solid wall can also enhance feelings of security [12][13].
Using Visual Schedules and Sensory Tools
While bedding supports physical comfort, visual aids can create a predictable and reassuring bedtime routine. A visual schedule that outlines steps like brushing teeth, using the bathroom, putting on pajamas, and getting into bed can provide structure and clarity. These tools are especially helpful for children aged 5 to 8, as they emphasize effort and progress rather than solely focusing on dry nights [2][3].
Incorporate sensory tools to create a calming atmosphere. Weighted blankets (used under professional guidance) or body pillows can offer grounding pressure that many children find soothing [12][13]. White noise machines or quiet fans can block out household sounds and provide a consistent background hum [12][14]. Keeping the room cool, around 65°F, also helps prevent overheating and supports restful sleep [14].
Lighting plays a crucial role in setting the mood. Replace harsh fluorescent bulbs with warm-toned LEDs or dimmable lights [12][13]. Blackout curtains can help manage light sensitivity, and if a nightlight is needed, choose one with amber or soft red tones to avoid disrupting sleep cycles [13]. Small nightlights in the bedroom and hallway can also make nighttime navigation easier and less intimidating.
Finally, keep dry pajamas and towels within easy reach. This not only makes cleanups more manageable but also encourages independence and reduces embarrassment for older children.
Conclusion
Bedwetting in children with autism presents a unique set of challenges, often tied to sensory differences, reduced bladder awareness, and difficulties with self-regulation. It's essential to understand that bedwetting is a medical condition, not a behavioral issue. This perspective shifts the focus from blame to support, encouraging patience and practical strategies that help reduce stress for both the child and their family [1]. The emotional and physical toll it takes on families highlights the importance of a thoughtful approach that includes predictable routines, sensory-friendly adjustments, and practical bedding solutions.
Addressing this issue effectively requires a mix of understanding and actionable tools. Products like PeelAways offer a practical solution that fits seamlessly into these strategies. With their peel-away design, PeelAways make overnight care significantly easier, eliminating the need for middle-of-the-night laundry while providing soft, breathable comfort [8]. Many caregivers emphasize how this simple yet effective solution helps reduce stress and maintain a sense of dignity for families navigating these challenges.
While most children eventually outgrow bedwetting, focusing on manageable factors - such as consistent routines and a calming sleep environment - can make the process less overwhelming. By combining structured habits with responsive bedding solutions, families can tackle bedwetting challenges with greater ease and confidence.
Related Articles
Check out these helpful resources for tackling bedwetting and caregiving challenges.
Managing Sensory Sensitivities in Children with Autism dives into creating a soothing bedtime environment by addressing sensory triggers like touch, sound, and smell. It offers practical tips, such as choosing noiseless waterproof bedding, using clear visual guides, and giving gradual time warnings (5, 2, and 1-minute intervals) to make the transition from play to bedtime smoother.
For guidance on toileting routines, Top Tips for Potty Training Kids with Special Needs provides structured strategies tailored for children on the autism spectrum. This guide complements the sensory and communication approaches mentioned earlier, featuring methods like the "Sit for Six" technique, using ASL for nonverbal cues, and celebrating small wins with positive reinforcement. Considering that roughly 1 in 54 children are diagnosed with autism[15], these tailored strategies can make potty training feel more manageable.
Lastly, How PeelAways Simplifies Bedding Changes for Caregivers highlights how their multi-layer bedding design eases the burden of nighttime accidents. Caregivers share how quickly a soiled layer can be removed - less than 60 seconds - without the need to strip the entire bed. This not only saves time but also helps preserve comfort and dignity for everyone involved[8].
FAQs
How can I create a bedtime routine that helps my child with autism feel calm and comfortable?
Establishing a calm and predictable bedtime routine can make a big difference for children with autism, helping them feel more secure and potentially reducing nighttime anxiety - and even bedwetting. One effective approach is to create a visual schedule that outlines each step of the routine. Include activities like brushing teeth, putting on pajamas, using the bathroom, and reading a bedtime story. Sticking to the same routine every night is crucial, as consistency helps children with autism feel more comfortable and in control.
Take time to adjust the sleep environment to suit your child’s sensory needs. For example, dim lighting or a soft-colored night-light can create a soothing atmosphere. Adding white noise or soft music can help block out unexpected sounds that might disrupt sleep. If your child is sensitive to textures, consider using a weighted blanket or soft, breathable pajamas to enhance their comfort.
Encouraging healthy bedtime habits can also play a role. Have your child use the bathroom twice before bed, limit evening fluids, and keep essentials like a clean set of pajamas and quick-change bedding close by. Products like Peelaways disposable bed sheets can simplify cleanup, making nighttime accidents less stressful for both you and your child. Pair these efforts with positive reinforcement, such as praise or small rewards, to help your child feel supported and confident in their bedtime routine.
When should I consult a doctor about my child’s ongoing bedwetting?
It’s wise to reach out to a doctor if your child is over 7 years old and still wets the bed, or if bedwetting happens at least twice a week for three months. Another red flag is sudden bedwetting after months of staying dry - this is known as secondary enuresis. Keep an eye out for other symptoms, such as painful urination, blood in the urine, foul-smelling urine, excessive thirst, frequent daytime accidents, constipation, fever, or back pain. These could point to an underlying medical issue that needs attention.
For children with autism, consulting a healthcare provider becomes even more crucial if bedwetting persists despite making routine adjustments or if any of these additional symptoms are present. Conditions like diabetes, bladder problems, or urinary tract abnormalities could be contributing factors. An early evaluation not only helps rule out medical causes but also ensures that treatments can be tailored to meet your child’s specific needs.
How can PeelAways disposable bed sheets help manage bedwetting in children with autism?
PeelAways disposable bed sheets provide an easy and hygienic way to handle bedwetting, especially for children with autism. These waterproof sheets are designed with a patented multi-layer system, offering 5 to 7 soft, absorbent layers depending on the size. When an accident occurs, simply peel off the top layer to reveal a fresh, clean sheet underneath - no need to lift the mattress, do laundry, or worry about cross-contamination.
Available in a variety of sizes, including crib, cot, Twin XL, and standard mattress dimensions, PeelAways accommodate toddlers to teens. The quick-change design minimizes cleanup stress, which is particularly beneficial for children who may be sensitive to changes in texture, disruptions to their routine, or strong odors. Caregivers appreciate how these sheets save time, keep beds dry, and help maintain a calm, consistent bedtime routine.
Comments
0

SAVE MONEY & WATER
Professionals & Institutions save a fortune on labor/laundry.

SUPERIOR COMFORT
The first thing our customers notice is how soft our sheets are.
100% WATERPROOF
Each layer is 100% Waterproof, perfect for spills and accidents

SAVE TIME
Change the sheet in under 1 minute without stripping the bed.




Leave a comment