How Pressure Relief Cushions Prevent Bed Sores

Pressure relief cushions are a key tool in preventing bed sores, also known as pressure ulcers. These cushions are designed to reduce pressure on sensitive areas, manage skin temperature, and control moisture - factors that contribute to the development of these painful injuries. Here's what you need to know:
- What They Do: Redistribute body weight, maintain blood flow, and protect skin from breakdown caused by pressure, friction, and moisture.
- Who Needs Them: Seniors, individuals with limited mobility, and those with conditions like diabetes or poor circulation are at higher risk.
-
Types Available:
- Foam: Affordable and effective for low-to-moderate risk.
- Gel: Helps with cooling and weight distribution.
- Air cushions: Alternating or static air designs for higher-risk users.
- Low Air Loss: Advanced systems for moisture and heat control.
Pairing these cushions with proper bedding, regular repositioning, and daily skin checks can significantly reduce the risk of sores. Consult a healthcare professional to choose the right cushion and care plan for individual needs.
What Are Bed Sores and Who Is at Risk
Defining Bed Sores
Bed sores, also known as pressure ulcers or decubitus ulcers, are injuries that affect the skin and underlying soft tissue. They usually develop over bony areas like the tailbone, hips, heels, ankles, elbows, shoulder blades, and even the back of the head. These sores occur when prolonged pressure disrupts blood flow to the area.
There are three main culprits behind bed sores: pressure, which compresses blood vessels; shear, where opposing forces stretch and damage vessels; and friction, which can rub and weaken the skin.
Bed sores can worsen quickly, progressing through four stages. In Stage 1, the skin appears red and doesn’t turn white when pressed. Stage 2 involves partial skin loss, often with blisters or shallow open wounds. By Stage 3, the damage extends deeper, forming a crater that reaches the fat layer. Stage 4 is the most severe, with the injury exposing muscle, tendons, or even bone, and significantly increasing the risk of severe infections like sepsis [2][6][7].
Understanding how these sores develop is the first step in recognizing why certain groups, particularly older adults, are more at risk.
Common Risk Factors
Older adults are especially vulnerable to bed sores due to several age-related changes. Their skin becomes thinner, less elastic, and loses protective fat layers. Prolonged immobility - whether caused by illness, injury, or recovery - further increases the risk. Chronic conditions like diabetes and heart disease also impair circulation and slow healing [5][2][7].
Another major factor is reduced sensation, often caused by nerve damage or neurological conditions. Without the ability to feel discomfort, individuals may not realize they need to change positions [2][7]. Incontinence is another risk, as constant exposure to moisture weakens the skin, making it more susceptible to breakdown [5][7]. Additionally, poor nutrition, especially low protein and calorie intake, reduces the body’s ability to heal and leaves less padding over bony areas. People with very little body fat who eat and drink minimally often have thinner, less resilient skin and poor circulation, compounding the problem [6][7].
Preventing and Treating Bed Sores - Alternating Pressure Pad
How Pressure Relief Cushions Work
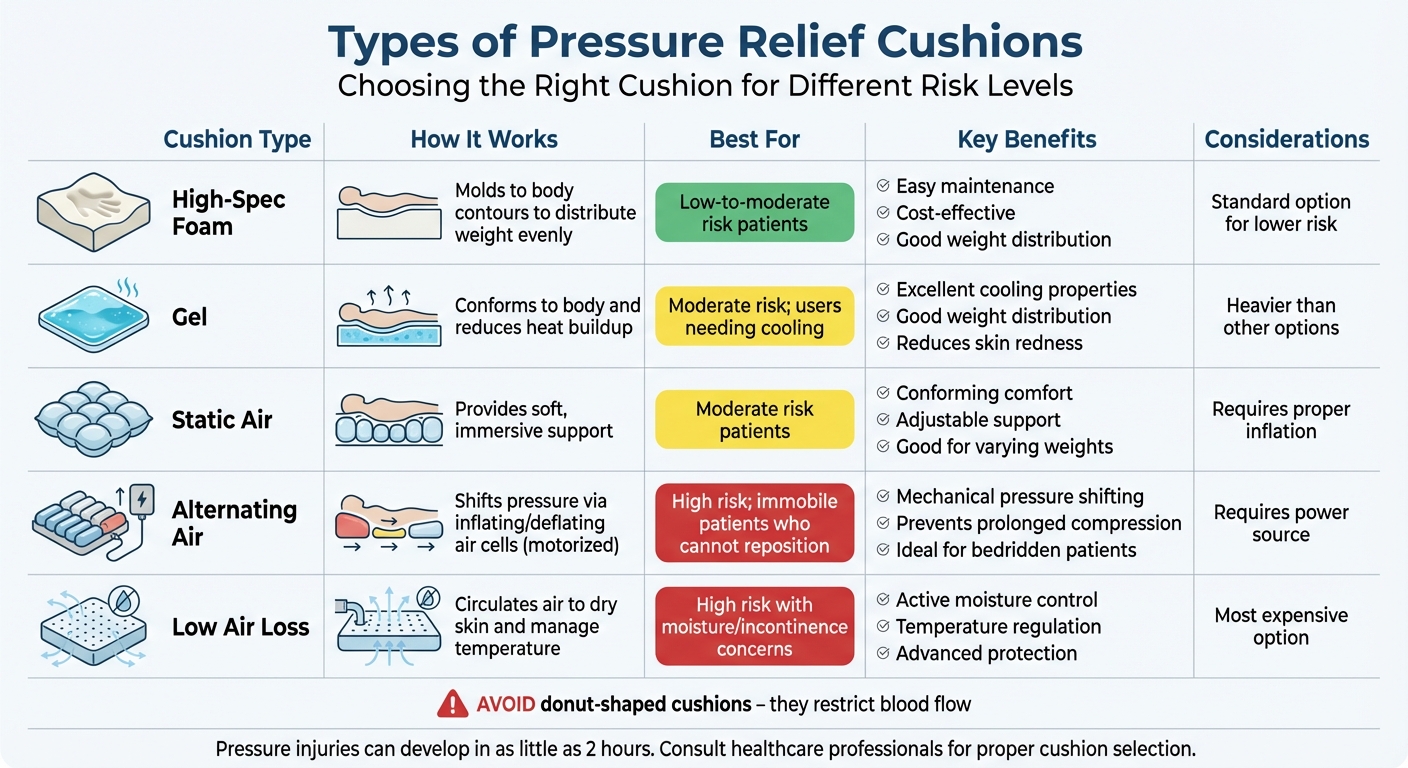
Types of Pressure Relief Cushions: Features and Best Uses Comparison Chart
Redistributing Body Weight
Pressure relief cushions are designed to spread body weight across a larger surface area, reducing the pressure on sensitive areas like the tailbone, hips, and heels [1][9].
"Pressure relief in a healthcare context means reducing the concentration of pressure on contact areas of the body when a patient is lying or sitting." – Vivid Care [9]
There are two main types of cushions that achieve this: Constant Low-Pressure (CLP) and Alternating-Pressure (AP) cushions. CLP cushions, typically made from foam or gel, adapt to the body’s shape, evenly distributing weight [9][10]. AP cushions, on the other hand, use motorized air cells that inflate and deflate in cycles, shifting pressure points periodically [3][9]. This process helps prevent blood vessel compression, ensuring that oxygen continues to flow to the skin tissues - an essential factor in maintaining healthy skin [6][9]. Without proper blood flow, pressure injuries can start forming in as little as two hours [4], making pressure redistribution a critical function.
But pressure relief cushions do more than just redistribute weight. They also play an important role in managing skin temperature and moisture to keep the skin healthy and protected.
Managing Skin Temperature and Moisture
Another key function of pressure relief cushions is controlling the skin’s microclimate, which includes temperature and moisture levels. Excessive heat and humidity can weaken the skin, increasing the risk of sores [9]. To combat this, many cushions incorporate features to regulate these factors. For example, gel-infused cushions and breathable covers, such as those made from Dartex fabric, enhance air circulation and help dissipate body heat [9][11]. For high-risk patients, Low Air Loss systems take it a step further by actively drying moisture from the skin’s surface [11].
By addressing both pressure redistribution and microclimate control, these cushions offer comprehensive protection against pressure sores.
Types of Pressure Relief Cushions
Pressure relief cushions come in a variety of designs, each tailored to different levels of risk and mobility requirements. Let’s break down the most common types:
- High-Specification Foam: These cushions contour to the body, offering effective weight distribution with minimal upkeep. They’re a great choice for those at low-to-moderate risk [10].
- Gel Cushions: Known for their cooling properties, gel cushions provide excellent weight distribution while helping to reduce heat buildup. However, they tend to be heavier [9][11].
- Static Air Cushions: These cushions offer soft, conforming support by allowing the user to "sink in", making them suitable for moderate-risk individuals [3][9][10].
- Alternating Air Cushions: Ideal for individuals who cannot reposition themselves, these cushions use air cells that inflate and deflate to shift pressure mechanically [3][9].
- Low Air Loss Cushions: Designed for high-risk users, these cushions circulate air to manage heat and moisture effectively [11].
One important tip: steer clear of donut-shaped cushions. While they might seem like a good idea, they can actually restrict blood flow to the center of the body and worsen sores [1][2][4].
Here’s a quick comparison of the key cushion types and their best applications:
| Cushion Type | How It Works | Best For |
|---|---|---|
| High-Spec Foam | Molds to body contours to distribute weight evenly | Low-to-moderate risk; easy maintenance |
| Gel | Conforms to the body and reduces heat buildup | Users needing cooling; moderate risk |
| Static Air | Provides soft, immersive support | Moderate risk; offers good comfort |
| Alternating Air | Shifts pressure via inflating/deflating air cells | High risk; immobile patients |
| Low Air Loss | Circulates air to dry skin and manage temperature | High risk with moisture concerns |
Choosing the Right Pressure Relief Cushion
When it comes to pressure relief cushions, picking the right one can make all the difference in providing comfort and preventing pressure sores.
Features to Look For
The material of the cushion plays a crucial role. For those at lower risk, high-density foam cushions are a practical and budget-friendly choice. If cooling and skin protection are priorities, gel cushions are a solid option - they help reduce skin redness but can be on the heavier side. For individuals at higher risk or with greater weight, air cell cushions offer adjustable support by redistributing air as the user moves, making them an ideal choice [13].
Size and fit are equally important, especially for wheelchair users. Always measure the seat’s length, width, and height to ensure the cushion provides proper coverage and stability. Experts recommend reassessing the fit annually - or more frequently if weight changes occur.
Don’t overlook the weight capacity of the cushion. Using a cushion that doesn’t support the user’s weight can lead to complete compression, rendering it ineffective [13]. For seniors dealing with incontinence, look for cushions with waterproof, zippered covers. These features not only protect the cushion but can also extend its lifespan to 3–5 years [13].
Working With Healthcare Professionals
If the individual is at high risk for pressure sores or already has them, consulting a healthcare professional is essential. Specialists like wound care experts, physical therapists, or doctors can recommend the best cushion type based on the person’s specific needs and the severity of any existing sores. A professional assessment ensures the cushion meets medical standards and could even help with insurance coverage [2][12].
"People at high risk of developing pressure ulcers should use higher-specification foam mattresses rather than standard hospital foam mattresses." – Elizabeth McInnes, School of Nursing, Midwifery and Paramedicine [10]
For those with Medicare, Medicare Part B covers 80% of the cost for pressure-reducing cushions once the deductible is met [12]. However, advanced surfaces like powered air flotation beds may require prior approval. A doctor’s prescription for "pressure-reducing support surfaces" can simplify the process and ensure the right equipment is obtained for the senior’s needs.
sbb-itb-45288fe
Using Cushions With Protective Bedding
Why Protective Bedding Matters
A pressure relief cushion is only as effective as the bedding that supports it. Clean, dry bedding plays a key role in managing skin moisture and minimizing friction, two critical factors in preventing pressure injuries [5]. While cushions redistribute weight, skin exposed to moisture - like sweat or other bodily fluids - becomes more susceptible to breakdown, even under reduced pressure [5]. This makes maintaining a stable and dry bedding environment essential.
Moisture and ill-fitting bedding can increase friction, weakening the skin's natural barrier [1][4]. This combination not only reduces the cushion's effectiveness but also raises the risk of severe complications, including cellulitis, bone infections, and even sepsis [4]. The takeaway? Smooth, clean, and dry bedding is a non-negotiable.
"When anything is placed between an individual and the cushion/mattress, surface tension is increased and thus they have a more difficult time immersing (sinking) into the cushion/mattress effectively." – PressureSoreCushions.com [14]
Another critical point is avoiding excessive layers - like thick towels or overly tight sheets - on top of the cushion. These layers can create a "hammock" effect, preventing the body from properly sinking into the cushion's pressure-relieving material [14]. To maximize the cushion's benefits, use minimal layers and ensure the bedding fits loosely. Specialized protective bedding can further enhance the effectiveness of pressure relief cushions.
PeelAways Disposable Fitted Sheets
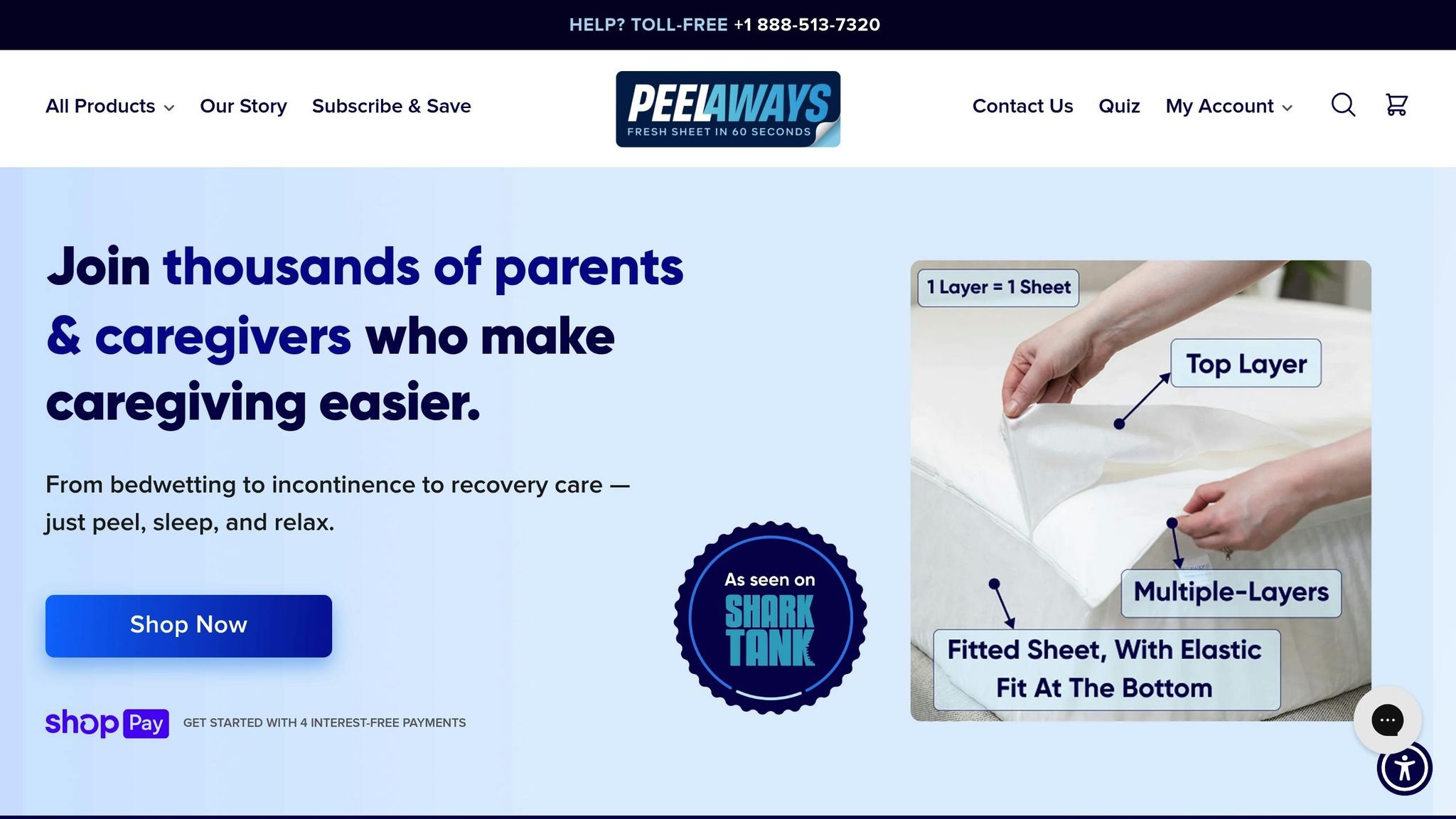
Specialized bedding, like PeelAways, offers a practical solution for caregivers dealing with incontinence or frequent bedding changes. These disposable fitted sheets are designed to work seamlessly with pressure relief cushions, featuring a patented multi-layer system with 5 to 7 soft, absorbent layers depending on the size. When a layer becomes soiled, you simply peel it away to reveal a fresh, clean sheet underneath - no need for mattress lifting, laundry, or worrying about cross-contamination.
The 100% waterproof material not only protects the mattress and cushion but also keeps the user's skin dry, a crucial factor in preventing moisture-related skin issues [5]. Unlike thick pads or tightly stretched sheets, PeelAways are thin and loosely fitted, ensuring they don’t interfere with the cushion’s ability to redistribute pressure effectively [14]. Available in sizes ranging from Crib and Cot to Twin XL (with 7 layers) and standard sizes like Twin, Full, Queen, and King, these sheets cater to a variety of needs, including elder care, medical recovery, special needs, and even potty training. They're chemical-free, breathable, and come with free shipping on orders over $100.
How To Use Pressure Relief Cushions Properly
Positioning the Cushion
Getting the positioning right is what makes a cushion effective. For wheelchair users, choose a foam or gel cushion that fits the wheelchair perfectly. Steer clear of donut-shaped or ring-shaped cushions - they actually restrict blood flow and can lead to sores instead of preventing them [1][2].
Before placing the cushion, make sure the bedding is dry, smooth, and free of objects like pins or coins [1]. Keep the head of the bed at a 30-degree angle or lower. This flatter position minimizes sliding, which helps avoid friction that can damage the skin [1][5]. If you use fitted sheets, secure them with sheet clips to keep the surface taut and smooth [15].
In bed, use pillows or foam to separate areas where the body presses against itself. For side-lying positions, place cushions between the knees and ankles [1][5]. For back-lying positions, add pillows under the tailbone, shoulders, shoulder blades, and elbows [1]. To protect the heels, position a pillow under the calves to lift the heels off the mattress - never place pillows directly under the knees, as this increases pressure on the heels [1].
| Positioning Need | Recommended Action |
|---|---|
| Wheelchair Support | Use foam or gel cushions; avoid donut shapes [1] |
| Side-Lying (Bed) | Place pillows between knees and ankles [1][5] |
| Back-Lying (Bed) | Place pillows under calves (to float heels), tailbone, and elbows [1] |
| Bed Angle | Keep it at 30 degrees or less to prevent sliding [1] |
Once the cushion is in place, regular checks are necessary to ensure it continues to provide protection.
Daily Monitoring and Repositioning
Repositioning isn’t optional - it’s critical. Wheelchair users need to shift their weight every 15–30 minutes for 30–90 seconds, while individuals confined to bed should change positions every 1–2 hours [1][8]. With proper care and repositioning, about 95% of pressure sores can be avoided [8].
Inspect the skin twice daily - once in the morning and again at bedtime - focusing on bony areas like the tailbone, hips, and heels [8][5]. Look for signs like redness, warmth, hardness, or changes in texture. Check seating surfaces daily for wear or sagging. To do this, slide your hand under the cushion while the person is seated; there should be enough padding between them and the chair surface [8].
Always lift, don’t drag. When transferring someone, lift them instead of dragging them across cushions or sheets to prevent friction-related skin tears [1][5]. Clean the skin immediately if there’s any incontinence, and change bedding right away - moist skin is much more prone to breakdown [8][5].
Daily care goes beyond just positioning; cleaning and maintenance are equally important.
Cleaning and Maintenance
Regular cleaning - at least once a week - helps prevent dirt, moisture, and bacteria from accumulating [17][18]. Wash outer covers in a washing machine at 104°F (40°C) with mild detergent, and let them air-dry completely before putting them back. Avoid using bleach, high-heat dryers, direct sunlight, or hairdryers [16][18][19].
Never submerge inner foam in water. If it gets wet, it may lose its functionality and should be replaced, especially if it’s contaminated by bodily fluids [16][17]. For air-filled cushions, close the air valve before cleaning and use vinegar or baking soda for deodorizing after washing [18]. Gel and fluid cushions should be cleaned by hand with soap and water - machine washing or drying is not an option [18].
"A well-maintained wheelchair cushion is key to skin protection, posture support, and overall comfort." – Nicole LaBerge, PT, ATP, Commercial Product Manager, Permobil Americas [17]
Before sitting, check the cushion for any sharp objects like keys or pens to avoid punctures [16][14]. Store cushions in a cool, dry place, away from temperatures below 41°F (5°C) or direct sunlight [16][19]. For gel cushions, regularly knead the material to keep it evenly distributed [17]. Most pressure relief cushions last between 2 and 5 years. Replace them if you notice permanent indentations, frequent air loss, or hardening [17].
Conclusion
Pressure relief cushions play a crucial role in preventing bed sores when used properly. They work by redistributing weight, maintaining healthy blood flow, and managing moisture - key factors in keeping skin intact and healthy.
However, choosing the right cushion is just the beginning. To maximize its effectiveness, daily skin checks, proper positioning, and regular cleaning are essential. Additionally, frequent weight shifting and repositioning are critical steps in preventing pressure injuries.
For even better results, pairing pressure relief cushions with moisture-controlling bedding, like PeelAways, can make a big difference. PeelAways' waterproof, multi-layer design not only helps keep the skin dry but also simplifies bedding changes, supporting the cushion's performance.
It’s always wise to consult a healthcare professional to determine the best cushion and repositioning schedule for individual needs. With over 3 million pressure injuries treated annually in the United States - costing the healthcare system an estimated $26.8 billion [20] - prevention is far more effective and less costly than treatment.
Related Articles
Dive into these articles for more strategies on preventing bed sores and improving elderly care. While focusing on the essentials like pressure relief and proper bedding, these resources offer a closer look at complementary aspects of care to enhance your approach.
How To Choose the Best Bedding for Elderly Care breaks down the types of mattresses and bedding materials that work well with pressure relief cushions. Learn how alternating pressure air mattresses can be a cost-efficient alternative to foam surfaces [21]. The article also covers tools like 30-degree side-lying wedges, which are effective in reducing pressure on vulnerable areas [22].
The Role of Moisture Control in Preventing Bed Sores highlights the importance of keeping skin dry. With pressure injuries in hospitals costing the U.S. healthcare system roughly $26.8 billion each year, this guide emphasizes the value of moisture barriers and proper cleansing techniques in prevention [20].
Top Tips for Caregivers Managing Incontinence tackles one of the toughest challenges for caregivers: managing incontinence while ensuring pressure relief cushions remain effective. This resource shares practical advice on layering protective bedding and maintaining skin health during frequent changes.
FAQs
How do pressure relief cushions help regulate skin temperature and moisture?
Pressure relief cushions are crafted to spread body weight evenly, which helps reduce pressure on the skin. They often include breathable materials that encourage airflow and pull moisture away from the skin. This design helps keep the skin cool and dry, cutting down on heat buildup and sweat - key factors in reducing the chances of skin irritation and bed sores.
What should I look for when choosing a pressure relief cushion for seniors?
When choosing a pressure relief cushion, it's important to start with the individual’s specific needs and health risks. Older adults with limited mobility, poor circulation, or conditions like diabetes or heart disease are at a higher risk for developing pressure sores. A cushion designed to evenly distribute weight and minimize pressure on sensitive areas - like the hips, tailbone, and heels - can make a big difference in preventing discomfort and skin issues.
Next, take a closer look at the materials and design options. Cushions made from foam, gel, air-filled cells, or hybrid combinations offer varying levels of support. The best choice often depends on the user’s unique requirements. For example, cushions that adapt to the body’s shape can reduce pressure points and provide better skin protection. Adjustable or layered designs are particularly useful for tailoring the cushion to the user’s comfort and support needs.
Lastly, don’t overlook practical considerations. Make sure the cushion fits the intended chair or bed, can support the user’s weight, and is easy to clean. Pairing it with waterproof bedding, like Peelaways disposable sheets, is a smart way to keep the skin dry and prevent moisture-related issues. And remember, regular repositioning and shifting weight are crucial steps in reducing the risk of developing pressure sores.
Why is it necessary to reposition someone even when using a pressure relief cushion?
Regular repositioning plays a crucial role in preventing bed sores because even the best pressure relief cushions can't completely eliminate all pressure on the skin. When pressure is sustained for too long, it can limit blood flow to certain areas, potentially leading to tissue damage and increasing the likelihood of bed sores. Shifting positions helps restore blood circulation, reduces friction, and gives the skin time to recover.
Moving someone every 1–2 hours - whether they're in bed or seated in a chair - helps relieve pressure on vulnerable areas. This gives stressed tissues a chance to heal and remain healthy. While cushions are a useful aid, frequent repositioning is the cornerstone of maintaining skin health and preventing sores.
Comments
0

SAVE MONEY & WATER
Professionals & Institutions save a fortune on labor/laundry.

SUPERIOR COMFORT
The first thing our customers notice is how soft our sheets are.
100% WATERPROOF
Each layer is 100% Waterproof, perfect for spills and accidents

SAVE TIME
Change the sheet in under 1 minute without stripping the bed.




Leave a comment