Incontinence Warning Signs: What Caregivers Should Know

Urinary incontinence affects at least 30% of people over 60 and is not an inevitable part of aging. Early detection and proper care can improve quality of life and prevent complications like infections, skin irritation, and emotional distress. Here’s what caregivers need to know:
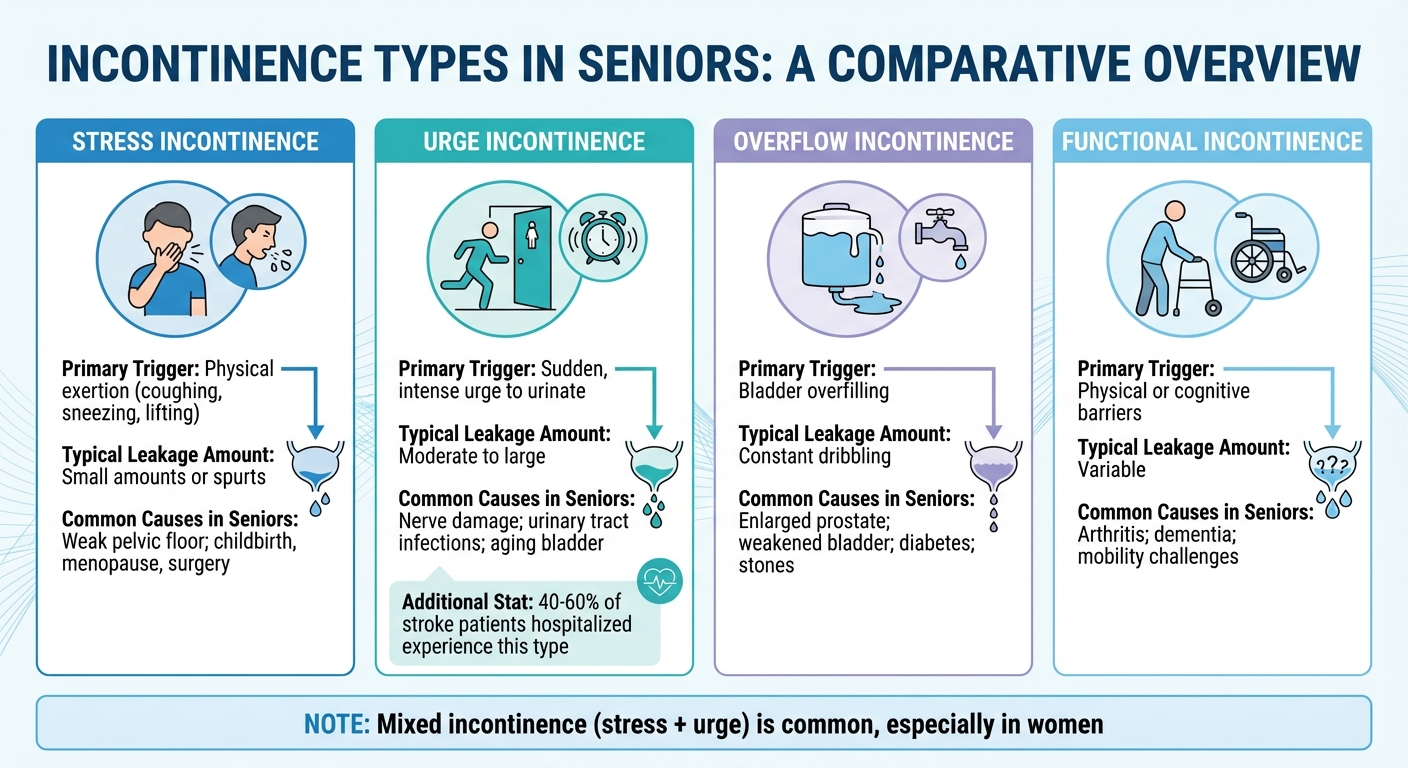
- Types of Incontinence: Stress, urge, overflow, and functional incontinence each have distinct causes and symptoms, such as leakage during physical activity or sudden urges to urinate.
- Warning Signs: Frequent urination, nocturia (waking up at night to urinate), or behavioral changes like avoiding social events may indicate incontinence.
- Common Causes: Aging-related muscle weakening, chronic conditions (e.g., diabetes, Parkinson’s), or medications can contribute to bladder control issues.
- Management Tips: Maintain hygiene, use absorbent products, create a bathroom schedule, and encourage pelvic exercises like Kegels.
Caregivers play a vital role in addressing incontinence with sensitivity, ensuring seniors receive timely medical attention and maintain their dignity.
Early Signs of Incontinence and when to Seek Help
4 Types of Incontinence in Seniors
4 Types of Incontinence in Seniors: Symptoms, Triggers, and Causes
Understanding the different types of incontinence is essential for caregivers and healthcare providers to offer the right support and discuss treatment options. Each type has its own triggers and symptoms, making it easier to identify and address the specific challenges seniors may face.
Stress Incontinence
Stress incontinence happens when physical pressure on the bladder causes urine leakage. This can occur during activities like coughing, sneezing, laughing, lifting heavy objects, or even standing up too quickly. Typically, the leakage involves small amounts of urine and happens without the sensation of needing to urinate beforehand.
The primary cause is weakened pelvic floor muscles or a damaged urethral sphincter, which struggles to keep urine contained. For women, this often stems from changes due to childbirth or menopause, while men may experience it after prostate surgery. As Harvard Health explains, "often only a small amount of urine leaks out [in stress incontinence]. In more severe cases, the pressure of a full bladder overcomes the body's ability to hold in urine." [9]
Urge Incontinence
Urge incontinence, commonly known as overactive bladder, is characterized by a sudden and strong urge to urinate, often leading to leakage before reaching the bathroom. Unlike stress incontinence, this urge comes on abruptly and can result in moderate to large amounts of urine being lost.
This condition is caused by involuntary bladder muscle contractions (detrusor overactivity). Common triggers include nerve damage, urinary tract infections, or age-related changes in bladder function. Research shows that between 40% and 60% of stroke patients hospitalized experience this type of incontinence. [9]
Overflow Incontinence
Overflow incontinence occurs when the bladder doesn’t empty completely, leading to overfilling and eventual leakage. Instead of sudden accidents, this type often involves constant or frequent dribbling of urine. Because the bladder remains partially full, urine may continuously seep out.
This form is more frequently seen in men, often due to an enlarged prostate (benign prostatic hyperplasia) that obstructs the urethra and disrupts normal urine flow. Other factors include a weakened bladder muscle, diabetes, or bladder stones, all of which can interfere with proper bladder emptying.
Functional Incontinence
Functional incontinence happens when physical or cognitive challenges prevent someone from reaching the bathroom in time, even though their bladder control is otherwise normal. According to the National Institute on Aging, "functional incontinence occurs in many older people who have normal bladder control. They just have a problem getting to the toilet because of arthritis or other disorders that make it hard to move quickly." [1]
Common barriers include severe arthritis that limits mobility, dementia that affects decision-making, or clothing that is difficult to remove quickly. Addressing functional incontinence often involves creating a clear, well-lit path to the bathroom and choosing clothing with simple, easy-to-manage fasteners.
| Incontinence Type | Primary Trigger | Typical Leakage Amount | Common Causes in Seniors |
|---|---|---|---|
| Stress | Physical exertion (e.g., coughing, sneezing, lifting) | Small amounts or spurts | Weak pelvic floor; childbirth, menopause, surgery |
| Urge | Sudden, intense urge to urinate | Moderate to large | Nerve damage; urinary tract infections; aging bladder |
| Overflow | Bladder overfilling | Constant dribbling | Enlarged prostate; weakened bladder; diabetes; stones |
| Functional | Physical or cognitive barriers | Variable | Arthritis; dementia; mobility challenges |
Mixed incontinence - where symptoms of both stress and urge incontinence are present - is also quite common, especially among women. Recognizing these types is the first step in identifying the warning signs, which will be explored next.
Warning Signs of Incontinence to Watch For
Recognizing the early signs of incontinence is crucial for maintaining independence and quality of life, especially for seniors. In the U.S., around 25 million people experience urinary incontinence, with half of women over 50 affected [13]. While the types of incontinence have already been outlined, it’s equally important to identify physical and behavioral changes that may signal its onset.
Physical Symptoms
Certain physical symptoms can serve as early indicators of incontinence. For example, minor urine leaks during everyday activities like coughing, sneezing, laughing, lifting, or bending often point to stress incontinence. On the other hand, a sudden, intense urge to urinate followed by an inability to reach the restroom in time suggests urge incontinence [10][12][13][4].
Frequent urination - defined as eight or more trips to the bathroom in a 24-hour period - can also indicate developing bladder control issues [12]. Similarly, needing to use the bathroom multiple times at night (nocturia) or experiencing bedwetting during sleep (nocturnal enuresis) are common warning signs [12][13]. Other symptoms to watch for include a weak urine stream, the sensation of incomplete bladder emptying, or constant dribbling of small amounts of urine [11][12][13].
If you notice more severe signs, such as blood in the urine, painful urination, or a complete inability to pass urine, these require immediate medical attention as they could signal serious underlying conditions [12].
In addition to physical symptoms, behavioral changes can often reveal the impact of incontinence on daily life.
Behavioral Changes
Behavioral shifts may be subtle at first but can offer important clues. For instance, seniors dealing with incontinence might start avoiding social activities like family gatherings, movie outings, or community events to prevent the embarrassment of an accident [8]. They may also limit their daily activities or refuse to leave home for extended periods, driven by the fear of being too far from a restroom [12][8].
"Older adults with urinary tract infections often seem agitated or more restless than usual." – Kristina Lubofsky, Gerontologist [15]
You might notice other signs, such as seniors hesitating to discuss toileting concerns or frequently checking for the nearest restroom. Some may even plan their entire schedule around bathroom access [12]. Sudden changes in mood or behavior - like confusion, agitation, or restlessness - could indicate a urinary tract infection, a condition that frequently triggers or worsens incontinence in older adults [15].
As Kristina Lubofsky explains, "As a family caregiver, be on the lookout for rapid or unexplained changes in mood or behavior, especially confusion or extreme fatigue" [15]. Recognizing these early signs can help ensure timely intervention, which will be explored further in the next section on management.
What Causes Incontinence in Seniors
Understanding the causes of incontinence is essential for addressing the underlying issues rather than just managing the symptoms. These causes range from medical conditions to daily habits, all of which play a role in influencing bladder control.
Medical Conditions
Many health conditions can lead to incontinence by disrupting the body's ability to regulate bladder function. Neurological disorders such as Parkinson's disease, multiple sclerosis, Alzheimer's disease, and strokes can damage the nerves responsible for signaling between the brain and bladder. This disruption makes it difficult to sense when it's time to urinate or control the release of urine. Additionally, diabetes can damage nerves and increase urine production, both of which contribute to bladder problems.
For men, an enlarged prostate (benign prostatic hyperplasia or BPH) can block the flow of urine and lead to an overactive bladder. In women, menopause-related estrogen loss and pelvic organ prolapse can weaken the pelvic floor and reduce tissue strength, making bladder control more challenging. Physical limitations caused by conditions like arthritis may also prevent seniors from reaching the bathroom in time.
Temporary issues such as urinary tract infections, vaginal infections, and severe constipation can also trigger sudden leakage. In these cases, incontinence often improves once the underlying problem is treated. It's worth noting that at least 1 in 10 people aged 65 or older experiences some form of incontinence [16].
Medications and Lifestyle Factors
Certain medications commonly prescribed to seniors can worsen bladder control. Diuretics, often referred to as "water pills", increase urine production, while antidepressants and sedatives can interfere with nerve signals or dull the body's ability to recognize a full bladder [6][4]. If incontinence begins after starting a new medication, it's important to discuss potential alternatives with a healthcare provider.
Diet and lifestyle choices also have a significant impact. Caffeine and alcohol act as bladder stimulants and diuretics, increasing both urgency and frequency. Obesity places constant pressure on the bladder and weakens pelvic floor muscles, while chronic constipation can cause the bowel to press against the bladder. Smoking contributes as well, with nicotine irritating the bladder walls and a chronic smoker's cough adding physical stress that can lead to stress incontinence.
Natural Aging Changes
Aging itself brings changes that can make seniors more prone to incontinence, even though aging alone isn't the direct cause. As noted by UCLA Health, "The most significant change is that the bladder becomes less elastic. That means it's no longer capable of holding as much urine as it used to" [17]. Reduced elasticity means the bladder feels fuller more quickly.
Older bladders also tend to contract more frequently, and these contractions become harder to control. Pelvic floor muscles weaken, making it harder to maintain bladder control during physical activity. The urinary sphincter, which keeps the urethra closed, may weaken or relax too easily due to bladder spasms. In men, the prostate gland often enlarges with age, compressing the urethra and making it difficult to fully empty the bladder. For women, hormonal changes after menopause can shorten the urethra and thin its lining, reducing the sphincter's ability to maintain a tight seal [17][5]. Over half of people aged 65 and older report experiencing some form of bladder or bowel incontinence [14].
sbb-itb-45288fe
When to Contact a Doctor
While occasional leaks might not be cause for concern, sudden changes or severe symptoms should never be ignored. Some situations call for immediate medical attention.
Warning Signs That Need Immediate Attention
Certain symptoms signal a medical emergency. If a senior experiences sudden bladder control loss along with difficulty speaking, walking, or moving, sudden weakness or numbness, vision loss, confusion, or loss of consciousness, call 911 right away [4].
"Call your local emergency number (such as 911) or go to an emergency room if you suddenly lose control over urine and you have: Difficulty talking, walking, or speaking; Sudden weakness, numbness, or tingling in an arm or leg; Loss of vision; Loss of consciousness or confusion." – MedlinePlus [4]
Also, seek urgent care if urinary retention occurs, which is the inability to urinate [12]. Other red flags include blood in the urine, burning or painful urination, fever, or pelvic pain combined with a full bladder [12]. Seniors with a history of stroke, spinal cord injury, or multiple sclerosis should report any sudden changes in urination patterns immediately [3].
For non-emergency situations, it's still important to consult a doctor if a senior urinates eight or more times a day, has a weak urine stream, experiences frequent bladder infections, or feels a strong urge but passes only small amounts of urine [12]. These symptoms may not be emergencies, but addressing them promptly can lead to better management and treatment.
How to Prepare for the Appointment
Being prepared for a doctor's visit can make a big difference in identifying the problem and finding effective solutions. Start by keeping a 24-hour bladder diary. Track fluid intake, bathroom visits, urine volume, and any leakage episodes. Note whether specific actions, like coughing or sneezing, seem to trigger leaks [18].
Bring a complete list of medications, including prescriptions, over-the-counter medicines, and supplements, as these can impact bladder function [4]. Write down any questions you have about managing symptoms, such as skin care, odor control, treatment options, or potential side effects. If possible, bring a family member or caregiver to help remember instructions and ask additional questions.
During the visit, the doctor will likely perform a physical exam, collect urine and blood samples, and use an ultrasound to check how well the bladder empties [1]. These steps are essential for determining the right course of action.
How to Manage Incontinence at Home
Once a doctor has assessed the situation, caregivers can take steps to manage incontinence effectively at home. A thoughtful mix of good hygiene practices, routine changes, and tweaks to the living space can make everyday life much easier.
Maintaining Hygiene and Comfort
Keeping the skin clean and healthy is a top priority. After every episode, clean the area right away to help prevent infections and irritation. Use warm water and a soft washcloth or a mild, fragrance-free perineal cleanser. Always wipe from front to back to avoid spreading bacteria [19]. Avoid harsh soaps or alcohol-based wipes, as they can dry out and irritate the skin [20].
Once the area is clean, gently pat the skin dry and, if possible, let it air dry for 5–10 minutes before putting on a new brief. To protect the skin from moisture, apply a barrier cream with ingredients like 10% zinc oxide, petroleum jelly, or lanolin [7].
Check incontinence products every three hours and replace them as soon as they become wet or soiled. Many modern products now include wetness indicators that change color when saturated, making it easier to know when it’s time for a change [19]. For bedding, consider PeelAways disposable sheets (starting at $30.99). These multi-layer sheets simplify cleanup by eliminating the need for mattress lifting or laundry, reducing the risk of cross-contamination [23].
Daily Routine Adjustments
Establishing a consistent bathroom schedule can help minimize accidents. Dr. Harvey Winkler, System Chief for Urogynecology at Northwell Health, suggests:
"Timed voiding - a fixed schedule for going to the bathroom - is a good way to keep the patient dry and reduce incontinence episodes" [22].
Plan bathroom visits every two hours during the day, especially after meals.
Proper hydration is also key. Aim for four to six glasses of water daily, as cutting back too much can lead to concentrated urine, which may irritate the bladder [2]. To reduce nighttime trips, limit fluids two to three hours before bed. Be mindful of bladder irritants like caffeine, alcohol, artificial sweeteners, chocolate, and acidic juices, which can worsen symptoms [2].
Encourage pelvic floor exercises, like Kegels, to strengthen the muscles that control urination. A basic routine involves squeezing for 10 seconds, relaxing for 10 seconds, and repeating this 15 times, three times a day [2]. For significant improvement, these exercises should be done 30 to 80 times daily for at least eight weeks [3]. For seniors with cognitive challenges, watch for nonverbal cues - like restlessness, pacing, or tugging at clothing - that may indicate the need to use the bathroom [21].
These daily adjustments work best when paired with a supportive and well-organized living space.
Setting Up a Helpful Living Space
An incontinence-friendly environment can ease stress and help with daily care. Protect mattresses with zippered vinyl waterproof covers, layering them with absorbent bed pads or disposable sheets like PeelAways [23]. Some caregivers even recommend using two waterproof covers for extra protection during heavy leaks [25].
Install grab bars near toilets or in stalls to provide stability. For seniors with mobility issues, keeping a bedside commode nearby can reduce the distance they need to travel during urgent moments [25]. Use absorbent pads or waterproof cushions on chairs, couches, and recliners to protect furniture [24].
Set up a dedicated changing station stocked with gloves, wipes, barrier cream, fresh briefs, and disposal bags for soiled items [7]. Keep the area fresh with urine odor neutralizers and proper ventilation, such as open windows or fans [24]. For outings, pack a "Plan B" bag with essentials like wipes, barrier cream, a full change of clothes, extra socks and shoes, and plastic bags for soiled items [25]. Consider clothing with elastic waistbands or Velcro fasteners to make dressing and undressing quicker and easier during urgent situations [21].
Conclusion: Caring for Seniors with Respect
Incontinence impacts at least 30% of people over 60 [2]. Recognizing the early signs and responding with empathy can go a long way in preserving a senior's dignity and emotional well-being. Addressing the issue early creates opportunities for effective and compassionate management.
It’s important to remember that incontinence, much like diabetes or high blood pressure, is manageable [2]. It’s not an unavoidable part of aging, nor should it be a source of shame. Approaching the topic with sensitivity and understanding helps seniors feel comfortable acknowledging the problem and exploring solutions such as bladder training, pelvic exercises, or medical treatments. Michele Mongillo, MSN, BSN, RN, Clinical Director at First Quality, highlights this sentiment:
"By writing this book, I hope to make hidden conversations more visible and help caregivers gain confidence in their ability to provide dignified care" [26].
Early detection is key to ensuring respectful and dignified care. Dignity begins with clear and considerate communication. Simple actions like closing doors, drawing blinds, or using blankets during care help maintain privacy [7]. Involving seniors in their care - by asking about their preferences, encouraging their input, and using discreet language - reinforces their sense of autonomy. As Parentgiving notes:
"You're seeing them in a very vulnerable situation, so it's best to be kind, open, communicative, respectful, and discreet" [7].
Practical steps can make daily life easier for both seniors and caregivers. Establishing a consistent bathroom schedule, using high-quality absorbent products (such as PeelAways disposable sheets), and prioritizing proper skin care can reduce accidents and enhance comfort. Ignoring incontinence can lead to a diminished quality of life [8]. Addressing it with care and understanding helps seniors maintain their independence, confidence, and overall well-being.
While caring for someone with incontinence can be challenging, a compassionate approach turns moments of vulnerability into opportunities for dignity, improving both daily comfort and emotional health.
Related Articles
Caring for seniors with incontinence goes beyond just recognizing the signs - it involves tackling everyday challenges like protecting bedding and maintaining hygiene. Here are some practical resources that offer actionable strategies to make caregiving easier and improve daily life.
How PeelAways Can Simplify Elder Care highlights a multi-layer peel-away system that eliminates the need to lift heavy mattresses and significantly reduces laundry time. With approximately 5 million U.S. adults experiencing bedwetting, tools like these are essential for maintaining dignity and easing the workload for caregivers.
Top Tips for Managing Bedwetting in Seniors offers practical advice for handling nighttime accidents. Strategies like limiting fluid intake before bed, elevating legs, and using high-absorbency overnight products can help reduce the frequency of accidents and improve sleep for both seniors and their caregivers.
The Role of Hygiene in Preventing Infections for Seniors emphasizes the importance of proper hygiene in preventing infections. Prolonged skin contact with urine can lead to bacterial and fungal infections [27]. This article covers essential cleaning techniques, the use of barrier creams, and setting optimal change schedules to protect seniors from conditions like incontinence-associated dermatitis and urinary tract infections.
FAQs
What are the early signs of urinary incontinence in older adults?
Early indicators of urinary incontinence in seniors can show up in subtle ways. You might spot damp spots on their clothing or furniture, or notice a persistent urine odor. Another common sign is frequent trips to the bathroom, particularly during the night. Seniors may also experience sudden, intense urges to urinate that are hard to manage.
Other clues include frequent changes of underwear or clothing, which could signal an attempt to manage accidents discreetly. In some cases, you might observe unexplained shifts in mood or behavior, possibly stemming from discomfort or feelings of embarrassment. Recognizing these signs early can make a big difference in providing the right care and support.
What are the best ways for caregivers to manage incontinence at home?
Managing incontinence at home begins with fostering open and empathetic conversations. Approach any accidents with understanding and reassurance, as feelings of embarrassment can often delay seeking help. It's crucial to consult a healthcare provider to pinpoint any underlying issues and explore possible treatments, such as bladder training, pelvic floor exercises, or medications.
Creating a regular toileting schedule - like every 2–3 hours and before bedtime - can help minimize accidents. To provide additional support, consider using well-fitting adult diapers or absorbent pads. Make sure to change them promptly to avoid skin irritation. After each change, clean the skin gently with warm water, apply a barrier cream to protect against moisture, and ensure the area is thoroughly dry.
For safeguarding bedding and furniture, PeelAways disposable, waterproof bed sheets offer a practical solution. Their multi-layer, peel-away design allows you to remove a soiled layer effortlessly, revealing a fresh one underneath - no heavy lifting or laundry required. Combine these with disposable underpads for extra protection on chairs or sofas, helping maintain a clean and comfortable environment for your loved one.
When should caregivers contact a doctor about a senior’s incontinence?
Caregivers should contact a doctor if a senior’s incontinence becomes so frequent or severe that it interferes with daily activities, leads to embarrassment, or causes them to withdraw socially. Medical advice is also crucial if incontinence increases the risk of falls, especially during urgent or nighttime trips to the bathroom.
It's essential to seek immediate medical attention if the senior shows signs like pain, fever, blood in their urine, or other symptoms of infection, as these could signal a more serious underlying health problem that needs prompt treatment.
Comments
0

SAVE MONEY & WATER
Professionals & Institutions save a fortune on labor/laundry.

SUPERIOR COMFORT
The first thing our customers notice is how soft our sheets are.
100% WATERPROOF
Each layer is 100% Waterproof, perfect for spills and accidents

SAVE TIME
Change the sheet in under 1 minute without stripping the bed.




Leave a comment